Sunday Poster Session
Category: Infections and Microbiome
P1356 - Triple Infection in an Immunosuppressed Host: CMV Colitis With Enteropathogenic E. coli Diarrhea and EBV Viremia
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Has Audio

Adlin Lawrence, MD
Orlando VA Medical Center and UCF/HCA Greater Orlando
Kissimmee, FL
Presenting Author(s)
Adlin Lawrence, MD1, Saud Khan, MD2, Ajay Desai, MD1, Luiz Fernando Sanchez, MD3, Jignesh Parikh, MD1
1Orlando VA Medical Center and UCF/HCA Greater Orlando, Kissimmee, FL; 2UCF/HCA Greater Orlando/Osceola, Kissimmee, FL; 3Orlando VA Medical Center and UCF/HCA Greater Orlando, Ki, FL
Introduction: Cytomegalovirus (CMV) is a significant complication in solid organ transplant recipients on immunosuppressive therapy. It can affect multiple organ systems, manifesting as colitis, hepatitis, retinitis, or disseminated disease. Prompt diagnosis and management are crucial to prevent poor outcomes. We present a complex case of CMV colitis in a kidney transplant recipient, complicated by concurrent enteropathogenic Escherichia coli (EPEC) diarrhea and Epstein–Barr virus (EBV) viremia.
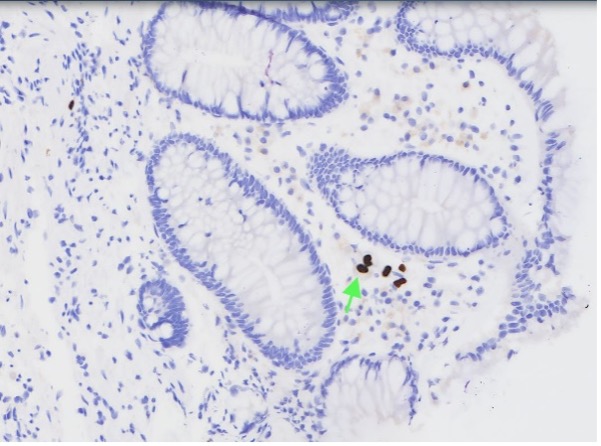
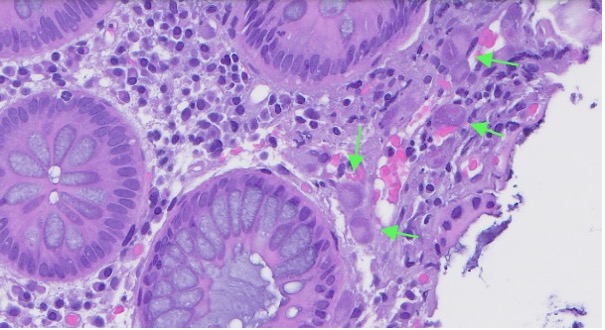
Case Description/Methods: A 68-year-old male with end-stage renal disease status post bilateral sequential kidney transplants, maintained on mycophenolate, belatacept, and low-dose steroids, presented with five days of non-bloody diarrhea and right upper quadrant pain. Laboratory evaluation showed elevated transaminases and CMV viremia exceeding 2,000,000 copies/mL. A GI multiplex panel detected EPEC. Initial imaging was unremarkable. On hospital day four, he developed hemodynamically significant gastrointestinal bleeding. Colonoscopy revealed patchy erythema, and biopsies confirmed CMV pancolitis via immunohistochemical staining. EBV viremia was also detected, raising concern for post-transplant lymphoproliferative disorder (PTLD), although no lymphoproliferative lesions were found. Subsequently, the patient developed bilateral CMV retinitis.
Treatment was initiated with intravenous ganciclovir due to the extent of viremia and tissue-invasive disease, later transitioning to oral valganciclovir. Belatacept was replaced with tacrolimus to reduce CMV risk. The patient improved with multidisciplinary care and was discharged with infectious disease follow-up.
Discussion: This case highlights the challenges of managing cytomegalovirus (CMV) infection in immunosuppressed transplant recipients, especially with multiorgan involvement and coinfections. Although enteropathogenic E. coli (EPEC) was initially suspected, the high CMV viral load and biopsy-proven pancolitis indicated CMV as the primary cause of diarrhea. Epstein–Barr virus (EBV) viremia suggested over-immunosuppression and raised concern for post-transplant lymphoproliferative disorder. Given literature associating belatacept with higher CMV and EBV risk, it was replaced with tacrolimus. Multidisciplinary management, including ganciclovir therapy and immunosuppressive adjustment, led to clinical improvement. This case underscores the need for early detection and tailored treatment in complex post-transplant scenarios.
Disclosures:
Adlin Lawrence, MD1, Saud Khan, MD2, Ajay Desai, MD1, Luiz Fernando Sanchez, MD3, Jignesh Parikh, MD1. P1356 - Triple Infection in an Immunosuppressed Host: CMV Colitis With Enteropathogenic <i>E. coli</i> Diarrhea and EBV Viremia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Orlando VA Medical Center and UCF/HCA Greater Orlando, Kissimmee, FL; 2UCF/HCA Greater Orlando/Osceola, Kissimmee, FL; 3Orlando VA Medical Center and UCF/HCA Greater Orlando, Ki, FL
Introduction: Cytomegalovirus (CMV) is a significant complication in solid organ transplant recipients on immunosuppressive therapy. It can affect multiple organ systems, manifesting as colitis, hepatitis, retinitis, or disseminated disease. Prompt diagnosis and management are crucial to prevent poor outcomes. We present a complex case of CMV colitis in a kidney transplant recipient, complicated by concurrent enteropathogenic Escherichia coli (EPEC) diarrhea and Epstein–Barr virus (EBV) viremia.
Case Description/Methods: A 68-year-old male with end-stage renal disease status post bilateral sequential kidney transplants, maintained on mycophenolate, belatacept, and low-dose steroids, presented with five days of non-bloody diarrhea and right upper quadrant pain. Laboratory evaluation showed elevated transaminases and CMV viremia exceeding 2,000,000 copies/mL. A GI multiplex panel detected EPEC. Initial imaging was unremarkable. On hospital day four, he developed hemodynamically significant gastrointestinal bleeding. Colonoscopy revealed patchy erythema, and biopsies confirmed CMV pancolitis via immunohistochemical staining. EBV viremia was also detected, raising concern for post-transplant lymphoproliferative disorder (PTLD), although no lymphoproliferative lesions were found. Subsequently, the patient developed bilateral CMV retinitis.
Treatment was initiated with intravenous ganciclovir due to the extent of viremia and tissue-invasive disease, later transitioning to oral valganciclovir. Belatacept was replaced with tacrolimus to reduce CMV risk. The patient improved with multidisciplinary care and was discharged with infectious disease follow-up.
Discussion: This case highlights the challenges of managing cytomegalovirus (CMV) infection in immunosuppressed transplant recipients, especially with multiorgan involvement and coinfections. Although enteropathogenic E. coli (EPEC) was initially suspected, the high CMV viral load and biopsy-proven pancolitis indicated CMV as the primary cause of diarrhea. Epstein–Barr virus (EBV) viremia suggested over-immunosuppression and raised concern for post-transplant lymphoproliferative disorder. Given literature associating belatacept with higher CMV and EBV risk, it was replaced with tacrolimus. Multidisciplinary management, including ganciclovir therapy and immunosuppressive adjustment, led to clinical improvement. This case underscores the need for early detection and tailored treatment in complex post-transplant scenarios.
Figure: Figure 1: Positive CMV immunohistochemical stain of colonic mucosa biopsy at 20x magnification
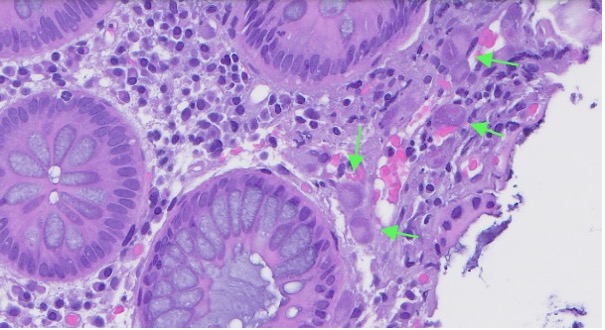
Figure: Figure 2: CMV inclusion bodies on H&E stain of colonic mucosa biopsy at 40x magnification
Disclosures:
Adlin Lawrence indicated no relevant financial relationships.
Saud Khan indicated no relevant financial relationships.
Ajay Desai indicated no relevant financial relationships.
Luiz Fernando Sanchez indicated no relevant financial relationships.
Jignesh Parikh indicated no relevant financial relationships.
Adlin Lawrence, MD1, Saud Khan, MD2, Ajay Desai, MD1, Luiz Fernando Sanchez, MD3, Jignesh Parikh, MD1. P1356 - Triple Infection in an Immunosuppressed Host: CMV Colitis With Enteropathogenic <i>E. coli</i> Diarrhea and EBV Viremia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
