Sunday Poster Session
Category: Colon
P0318 - Inpatient Clostridiodes difficile Disposition and Isolation: A Performance Metrics and a Quality Improvement Project
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Has Audio

Karan J. Yagnik, MD
Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University
Long Branch, NJ
Presenting Author(s)
Karan J.. Yagnik, MD1, FNU Payal, MD1, Anoohya Vangala, MD1, Malay Rathod, MD1, Sandeep Kotnani, MD1, Rutuja Challawar, MD1, Aayushi Parikh, BA2, Alysta Paneque, BA2, Wael Ghali, MD1
1Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: Clostridioides difficile (C. diff) is a highly contagious infection affecting over 500,000 individuals annually, with 30,000 deaths. CDC guidelines recommend initiating contact isolation when C. diff is suspected. At our hospital, isolation is triggered automatically when a C. diff test is ordered. However, tests are often ordered after just 1–2 loose stools, sometimes in patients on stool softeners, leading to potentially unnecessary isolation and delayed dispositions—particularly in the ED—impacting hospital flow and metrics. This quality improvement (QI) project evaluates the appropriateness of holding patient disposition and initiating isolation solely based on C. diff test orders, aiming to assess whether physicians can override these holds when clinical suspicion is low.
Methods: We conducted a retrospective EHR review of C. difficile test orders from 08/11/24 to 09/10/24. Each case was assessed for alternative diagnoses, prior C. diff history, and risk factors. Physician documentation was reviewed to determine if C. diff was an active clinical consideration. Positive PCR and/or toxin tests confirmed diagnosis. Descriptive analysis was performed using Microsoft Excel.
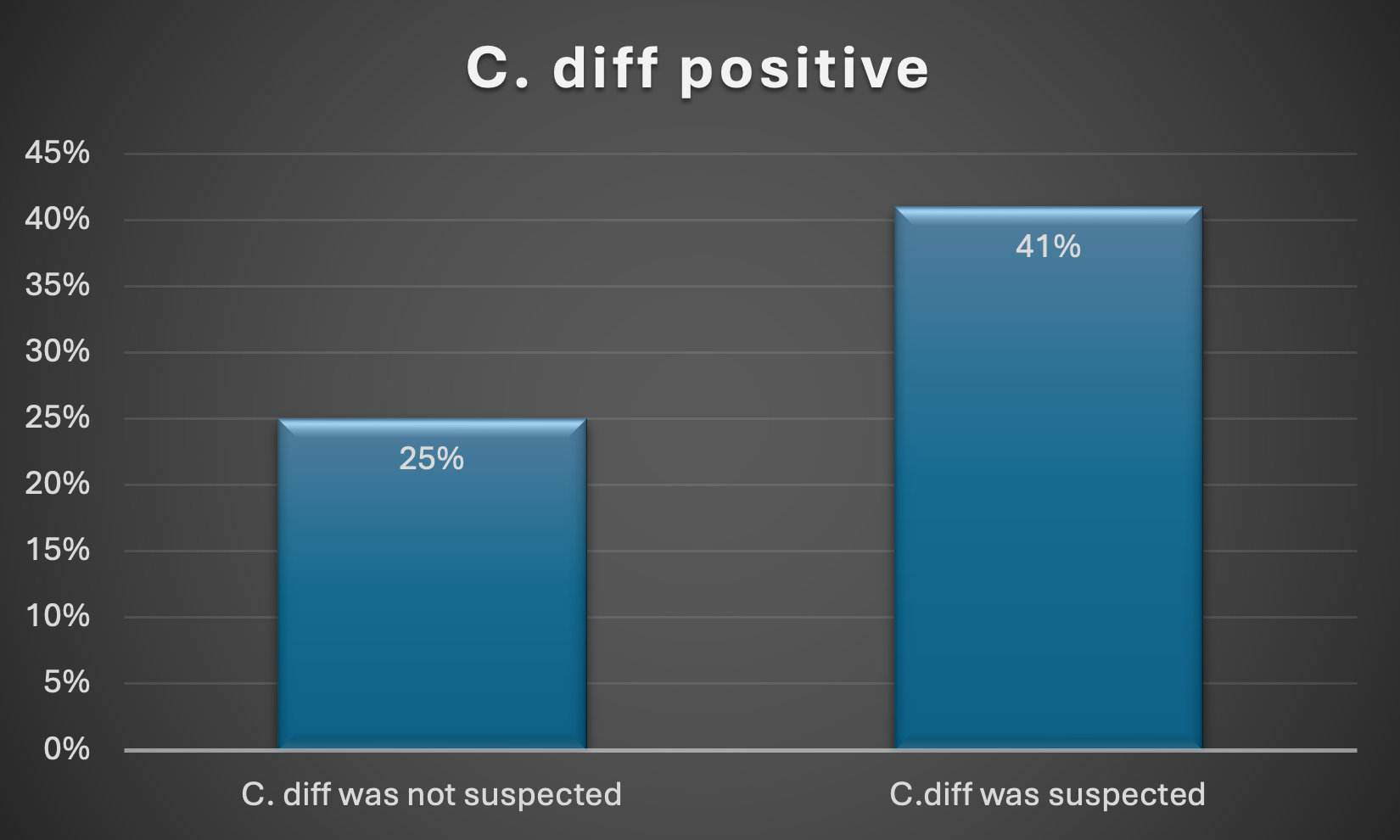
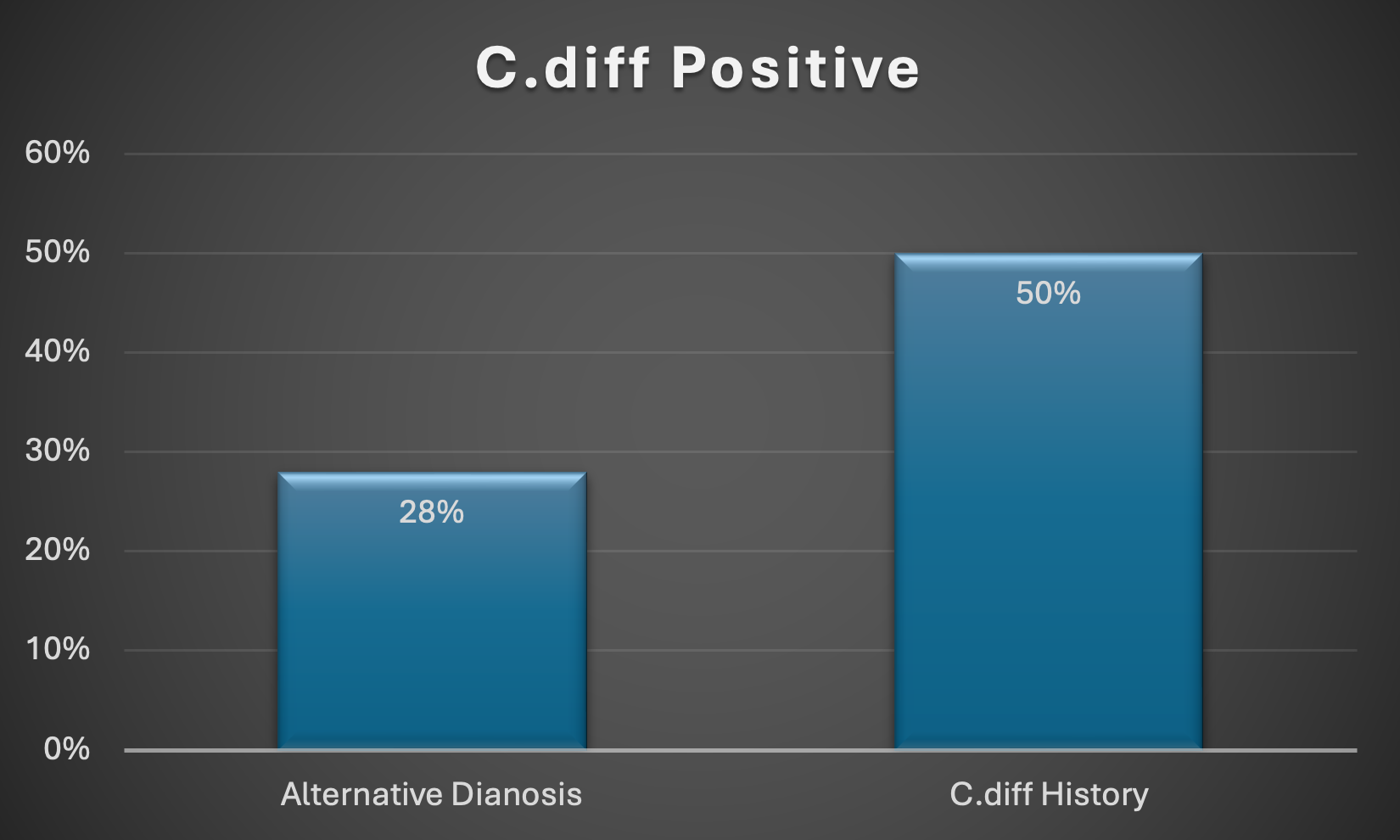
Results: A total of 93 patients with C. diff test orders were identified during the study period, with two excluded due to unclear or insufficient documentation. Of the remaining cases, 59 (65%) showed that providers were actively considering C. diff as a diagnosis. Risk factors were present in 65 (71%) patients, 72 (79%) had a potential alternative diagnosis, and only 8 (9%) had a prior history of C. diff. Providers correctly suspected C. diff in 24 (41%) cases, while 8 (25%) cases were not initially suspected (<em>Figure 1</em>). Interestingly, 20 (28%) patients diagnosed with C. diff had clinical notes suggesting an alternative diagnosis, and only 4 (50%) C. diff-positive patients had a prior history of the infection (<em>Figure 2</em>).
Discussion: Our study suggests that providers often face challenges in accurately predicting C. diff infections based on patient history, symptoms, and previous infections. When a C. diff test is ordered, the patient should be placed in isolation right away. If the patient is in a shared room, arrangements should be made for their transfer to a private room. While patient flow is a critical metric in the emergency department, if a C. diff order is placed, it is essential to temporarily pause disposition until a private room becomes available for the patient's safety.
Disclosures:
Karan J.. Yagnik, MD1, FNU Payal, MD1, Anoohya Vangala, MD1, Malay Rathod, MD1, Sandeep Kotnani, MD1, Rutuja Challawar, MD1, Aayushi Parikh, BA2, Alysta Paneque, BA2, Wael Ghali, MD1. P0318 - Inpatient <i>Clostridiodes difficile</i> Disposition and Isolation: A Performance Metrics and a Quality Improvement Project, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: Clostridioides difficile (C. diff) is a highly contagious infection affecting over 500,000 individuals annually, with 30,000 deaths. CDC guidelines recommend initiating contact isolation when C. diff is suspected. At our hospital, isolation is triggered automatically when a C. diff test is ordered. However, tests are often ordered after just 1–2 loose stools, sometimes in patients on stool softeners, leading to potentially unnecessary isolation and delayed dispositions—particularly in the ED—impacting hospital flow and metrics. This quality improvement (QI) project evaluates the appropriateness of holding patient disposition and initiating isolation solely based on C. diff test orders, aiming to assess whether physicians can override these holds when clinical suspicion is low.
Methods: We conducted a retrospective EHR review of C. difficile test orders from 08/11/24 to 09/10/24. Each case was assessed for alternative diagnoses, prior C. diff history, and risk factors. Physician documentation was reviewed to determine if C. diff was an active clinical consideration. Positive PCR and/or toxin tests confirmed diagnosis. Descriptive analysis was performed using Microsoft Excel.
Results: A total of 93 patients with C. diff test orders were identified during the study period, with two excluded due to unclear or insufficient documentation. Of the remaining cases, 59 (65%) showed that providers were actively considering C. diff as a diagnosis. Risk factors were present in 65 (71%) patients, 72 (79%) had a potential alternative diagnosis, and only 8 (9%) had a prior history of C. diff. Providers correctly suspected C. diff in 24 (41%) cases, while 8 (25%) cases were not initially suspected (<em>Figure 1</em>). Interestingly, 20 (28%) patients diagnosed with C. diff had clinical notes suggesting an alternative diagnosis, and only 4 (50%) C. diff-positive patients had a prior history of the infection (<em>Figure 2</em>).
Discussion: Our study suggests that providers often face challenges in accurately predicting C. diff infections based on patient history, symptoms, and previous infections. When a C. diff test is ordered, the patient should be placed in isolation right away. If the patient is in a shared room, arrangements should be made for their transfer to a private room. While patient flow is a critical metric in the emergency department, if a C. diff order is placed, it is essential to temporarily pause disposition until a private room becomes available for the patient's safety.
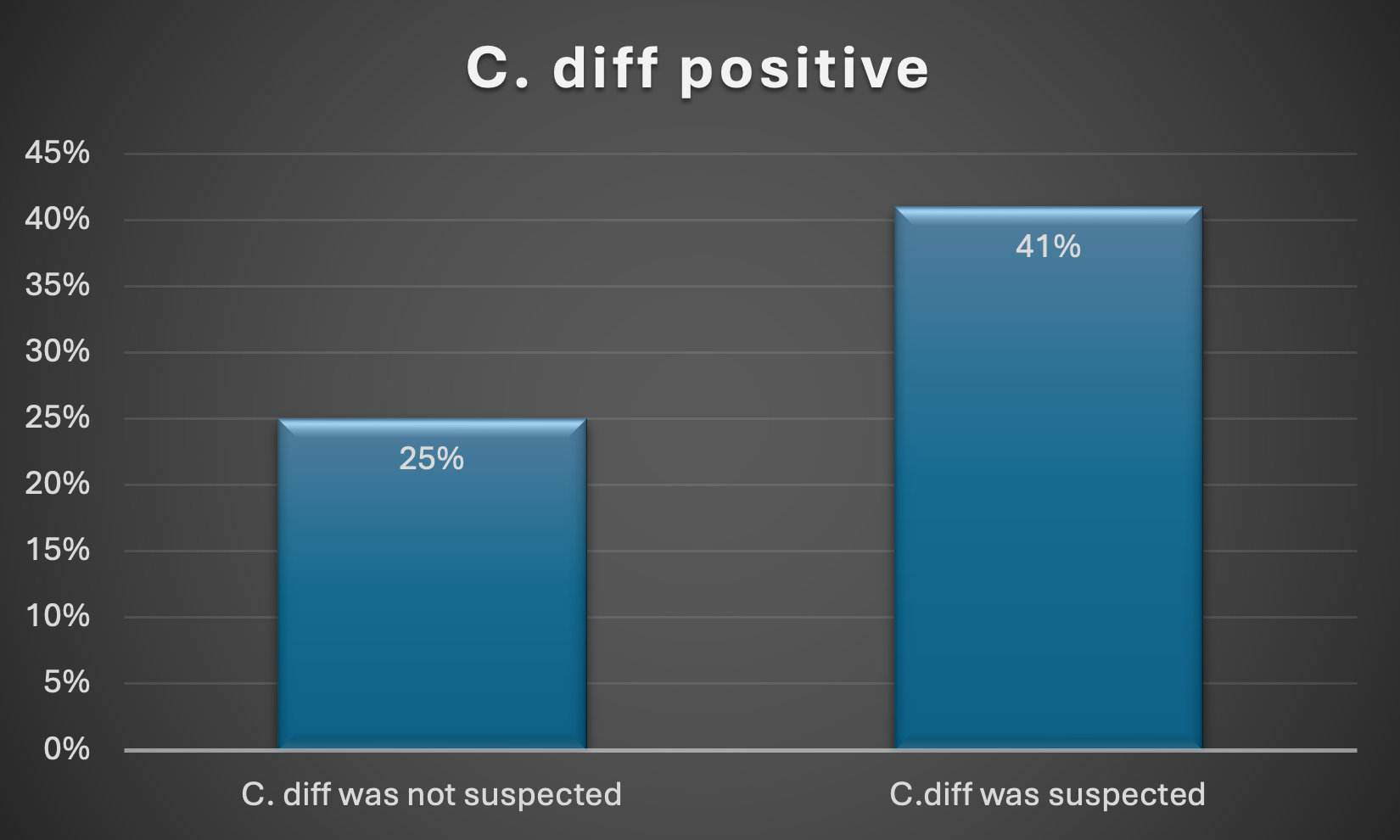
Figure: C. diff positive when C. diff Suspected vs C. diff not suspected.
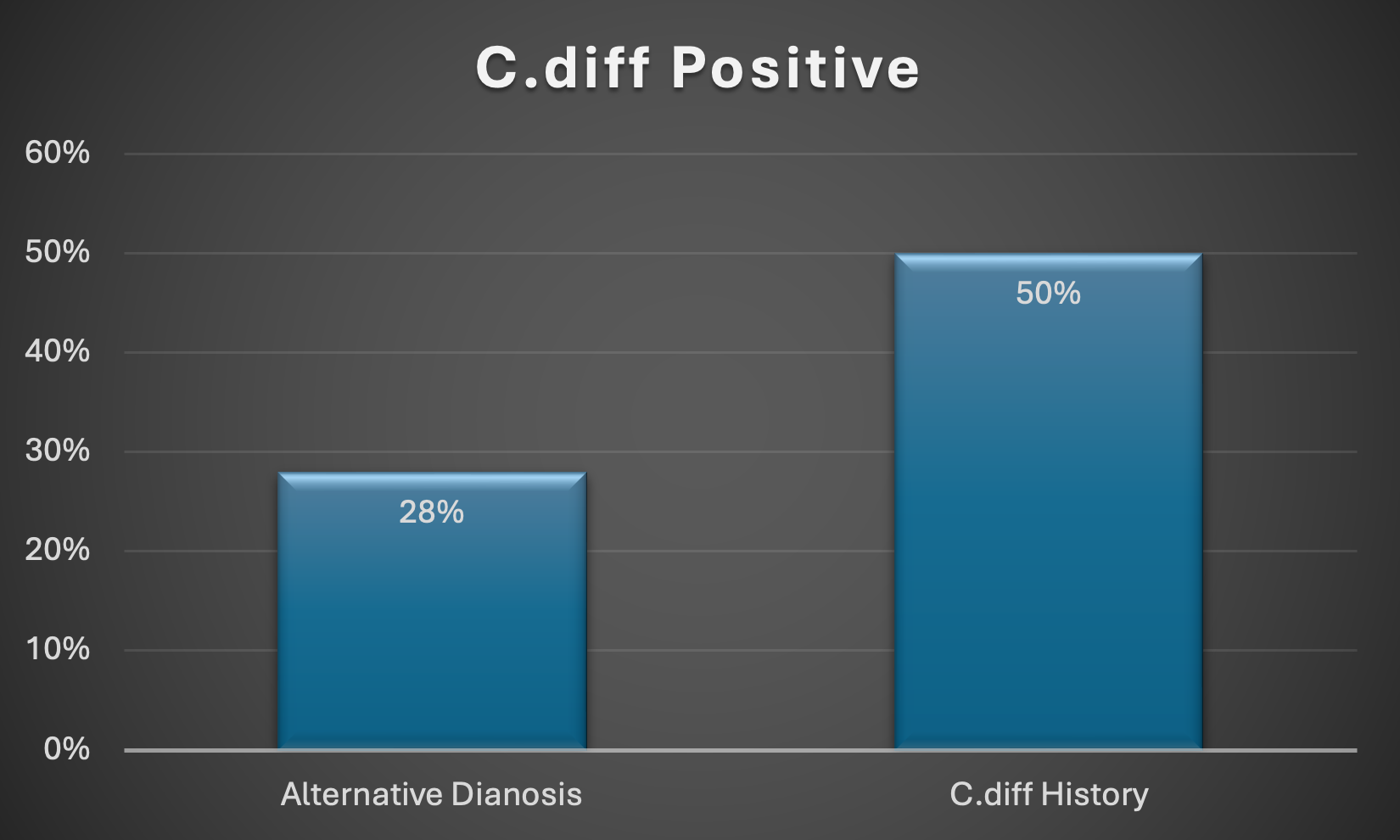
Figure: C. diff Positive results in alternative suspicion and past medical history of C. diff.
Disclosures:
Karan Yagnik indicated no relevant financial relationships.
FNU Payal indicated no relevant financial relationships.
Anoohya Vangala indicated no relevant financial relationships.
Malay Rathod indicated no relevant financial relationships.
Sandeep Kotnani indicated no relevant financial relationships.
Rutuja Challawar indicated no relevant financial relationships.
Aayushi Parikh indicated no relevant financial relationships.
Alysta Paneque indicated no relevant financial relationships.
Wael Ghali indicated no relevant financial relationships.
Karan J.. Yagnik, MD1, FNU Payal, MD1, Anoohya Vangala, MD1, Malay Rathod, MD1, Sandeep Kotnani, MD1, Rutuja Challawar, MD1, Aayushi Parikh, BA2, Alysta Paneque, BA2, Wael Ghali, MD1. P0318 - Inpatient <i>Clostridiodes difficile</i> Disposition and Isolation: A Performance Metrics and a Quality Improvement Project, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
