Sunday Poster Session
Category: Colon
P0328 - Henoch-Schönlein Purpura Mimicking Inflammatory Bowel Disease: A Case of Chronic Colitis in an Adolescent With Iga Vasculitis
Abel Sanchez, MD, MSc
Hospital Roosevelt / Gastri-k
Guatemala City, San Marcos, Guatemala
Presenting Author(s)
Yuli Toledo, 1, Abel Sanchez, MD, MSc2
1Gastroenterology an Digestive Endoscopy, Hospital Roosevelt, Guatemala, Guatemala City, Chimaltenango, Guatemala; 2Hospital Roosevelt / Gastri-k, Guatemala City, San Marcos, Guatemala
Introduction:
Henoch-Schönlein Purpura (HSP), or IgA vasculitis, is the most common systemic vasculitis in children and adolescents. Gastrointestinal involvement is common but rarely mimics inflammatory bowel disease (IBD). We report a rare case of an adolescent presenting symptoms suggestive of ulcerative colitis (UC) but ultimately diagnosed with IgA vasculitis
Case Description/Methods:
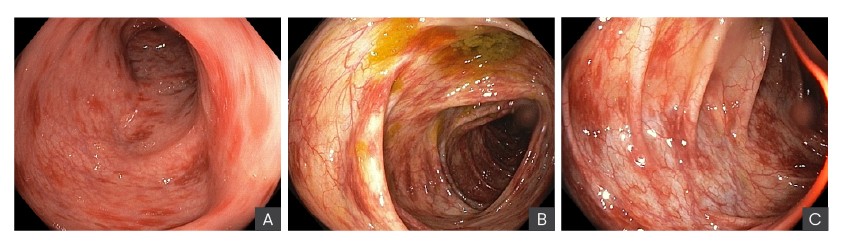
A 17-year-old female presented with a 1-day history of hematochezia accompanied by nausea and generalized abdominal pain (7/10 intensity). She reported over 10 episodes of hematochezia within 24 hours. Stool cultures for Clostridium difficile, Salmonella spp., Staphylococcus aureus, Escherichia coli, CMV, and HIV was all negative. One week earlier, she had been evaluated for purpuric skin lesions on her lower extremities and polyarthralgia. A skin biopsy revealed granular IgA deposition, consistent with IgA vasculitis Colonoscopy revealed diffuse mucosal erythema and erosions throughout the colon, with representative findings from the rectum, descending colon, and splenic flexure; Additionally, discrete ulcers measuring approximately 1 cm in diameter were noted in the sigmoid colon and cecum. The terminal ileum appeared endoscopically normal. These findings initially raised concern for ulcerative colitis. Histological examination of colonic biopsy samples showed mucosal congestion with dense infiltration of lymphocytes, plasma cells, and neutrophils. However, when correlated with the extraintestinal manifestations and the skin biopsy findings, the diagnosis of gastrointestinal involvement in Henoch-Schönlein Purpura (IgA vasculitis) was established. The patient responded favorably to systemic corticosteroid therapy, with complete resolution of gastrointestinal symptoms after two weeks of treatment
Discussion:
IgA vasculitis can mimic inflammatory bowel disease, especially when gastrointestinal symptoms dominate the clinical picture. In this case, endoscopic and histologic features suggested ulcerative colitis; however, the presence of extraintestinal symptoms and IgA deposits was crucial in identifying the true etiology. Differentiating vasculitis from IBD is essential, as treatment and prognosis differ. Prompt recognition and steroid therapy led to complete symptom resolution in this patient
Disclosures:
Yuli Toledo, 1, Abel Sanchez, MD, MSc2. P0328 - Henoch-Schönlein Purpura Mimicking Inflammatory Bowel Disease: A Case of Chronic Colitis in an Adolescent With Iga Vasculitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

