Sunday Poster Session
Category: Colon
P0332 - Acute Appendicitis or Something More? High-Grade B-Cell Non-Hodgkin’s Lymphoma Presenting as Appendicitis in a Young Adult

Abby Kunitsky, DO
McLaren Macomb
Mt. Clemens, MI
Presenting Author(s)
1Corewell Health, Farmington Hills, MI; 2McLaren Macomb, Mt. Clemens, MI
Introduction:
Primary appendiceal lymphomas are rare, accounting for < 1% of gastrointestinal lymphomas. They often present as acute appendicitis, with diagnosis typically made postoperatively via histopathology. We present a case of a young male diagnosed with high-grade B-cell non-Hodgkin’s lymphoma, not otherwise specified (HGBL-NOS) of the appendix following laparoscopic appendectomy.
Case Description/Methods:
A 25-year-old male presented with 24 hours of abdominal pain, nausea, and vomiting. Exam revealed percussive tenderness, guarding, and rigidity. Labs were notable for leukocytosis (15.8×109/L) and elevated CRP (445 mg/L). CT abdomen/pelvis with IV contrast demonstrated an inflamed tubular structure extending from the cecum, 5.9 cm abscess formation, and mesenteric lymphadenopathy (Figure 1). Laparoscopic appendectomy revealed a necrotic, ruptured appendix adherent to the terminal ileum. Histopathology showed sheets of lymphoma cells with a starry-sky pattern, high Ki-67 index (~100%), and immunophenotypic features consistent with HGBL-NOS (Figure 2, 3). PET/CT revealed FDG-avid mesenteric lymph nodes without distant metastasis, and bone marrow biopsy was negative. The patient was initiated on systemic R-CHOP chemotherapy.
Discussion:
Primary appendiceal lymphoma is an exceedingly rare GI malignancy (0.015% of GI lymphomas), often mimicking acute appendicitis. Gastroenterologists play a key role in recognizing atypical CT findings, including a bulky, homogeneously enhancing appendiceal mass with mesenteric lymphadenopathy, which may suggest lymphoma rather than typical appendicitis. In such cases, early gastroenterology consultation can guide further evaluation, including colonoscopy to assess for synchronous GI involvement or endoscopic ultrasound (EUS) if an appendiceal mass is detected.
Histopathology confirmed HGBL-NOS in our case, an aggressive but treatable malignancy. Although surgery addressed the acute disease, ongoing gastroenterology surveillance is crucial for recurrence or secondary GI involvement. This case underscores the importance of histopathologic evaluation of appendectomy specimens and the need for gastroenterologists to recognize atypical presentations of GI malignancies, as early suspicion may influence evaluation options, prognosis, and long-term management.

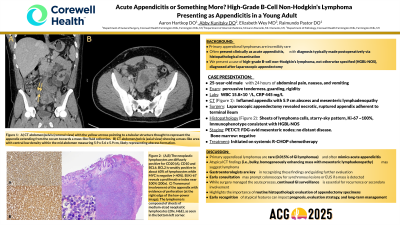
A) CT scan of the abdomen/pelvis (coronal plane) with the yellow arrows pointing to a tubular structure thought to represent the appendix extending from the cecum towards a mass-like fluid collection.
B) CT scan of the abdomen/pelvis (axial plane) showing a mass-like area with central low density within the mid abdomen measuring 5.9 x 5.6 x 5.9 cm, likely representing abscess formation.
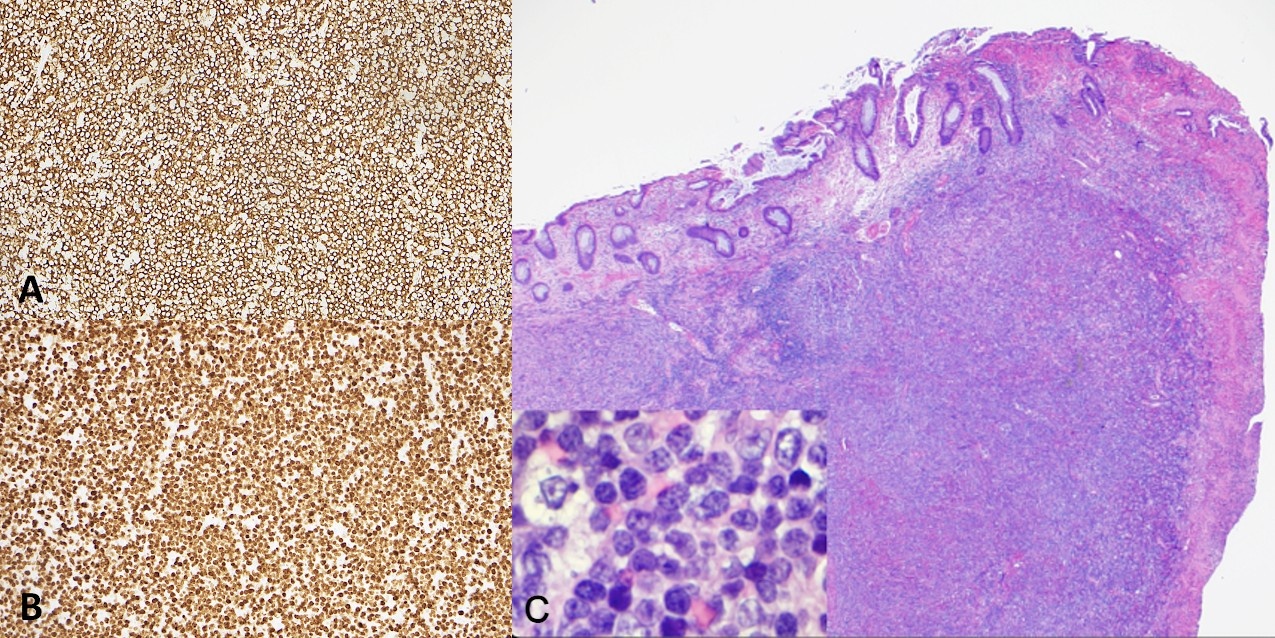
A) The neoplastic lymphocytes are diffusely positive for CD20 (A), CD10 and BCL6. BCL2 is weakly positive in about 60% of lymphocytes while MYC is negative (<40%).
B) Ki-67 reveals a proliferative index near 100% (200x).
C) H&E composite image demonstrating transmural involvement of the appendix with evidence of perforation (area of perforation at the right edge of the low-power image). The lymphoma is composed of sheets of medium sized neoplastic lymphocytes (20x, H&E), as seen in the bottom left corner.
Disclosures:
Aaron Hartkop, DO1, Abby Kunitsky, DO2, Elizabeth Wey, MD1, Raimundo Pastor, DO1. P0332 - Acute Appendicitis or Something More? High-Grade B-Cell Non-Hodgkin’s Lymphoma Presenting as Appendicitis in a Young Adult, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
