Sunday Poster Session
Category: Colon
P0338 - Medullary Carcinoma of the Transverse Colon in a Medically Complex Elderly Patient

Sunny Kumar, MD
Wright Center for Graduate Medical Education
Scranton, PA
Presenting Author(s)
1Wright Center for Graduate Medical Education, Scranton, PA; 2North Central Bronx Hospital, Bronx, NY; 3Northwell Health, Port Jefferson, NY; 4Ascension Saint Joseph Hospital, Chicago, IL; 5Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 6Geisinger Health System, Danville, PA
Introduction:
Medullary carcinoma of the colon is a rare histologic subtype of colorectal cancer, accounting for < 1% of all cases. It typically affects elderly women and arises in the right colon. Diagnosis requires histopathology and immunohistochemistry, with MSI testing guiding potential immunotherapy use. Here we present an unusual case of medullary carcinoma in the transverse colon, which was found incidentally.
Case Description/Methods:
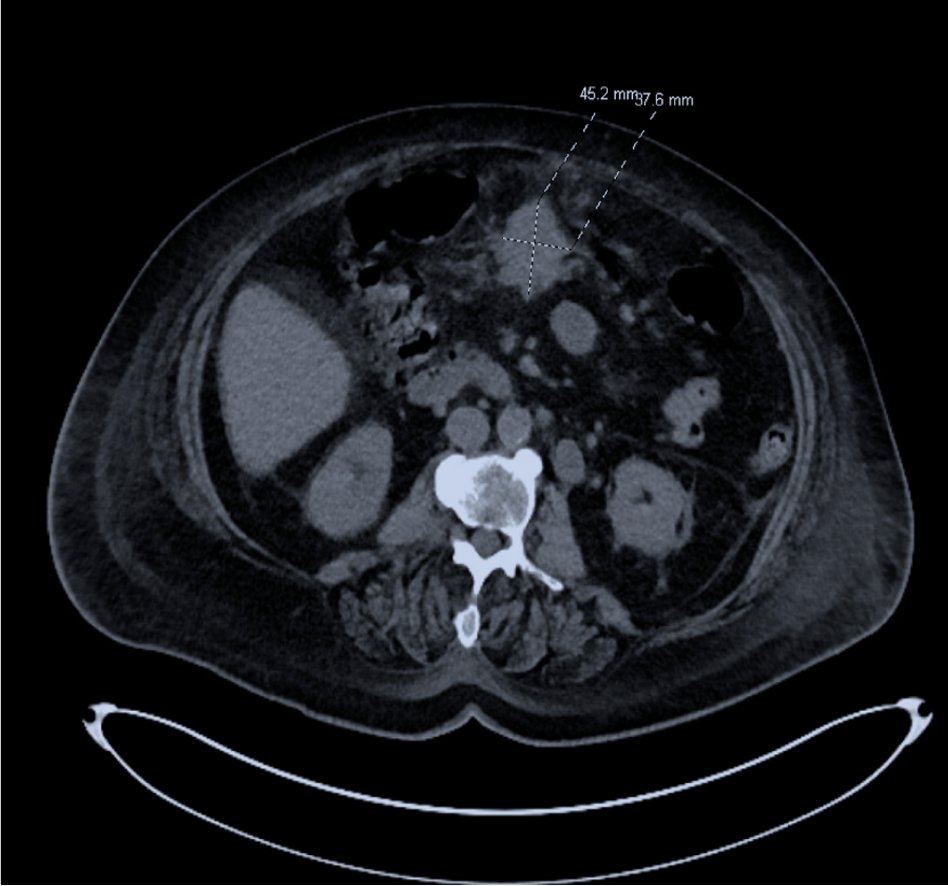
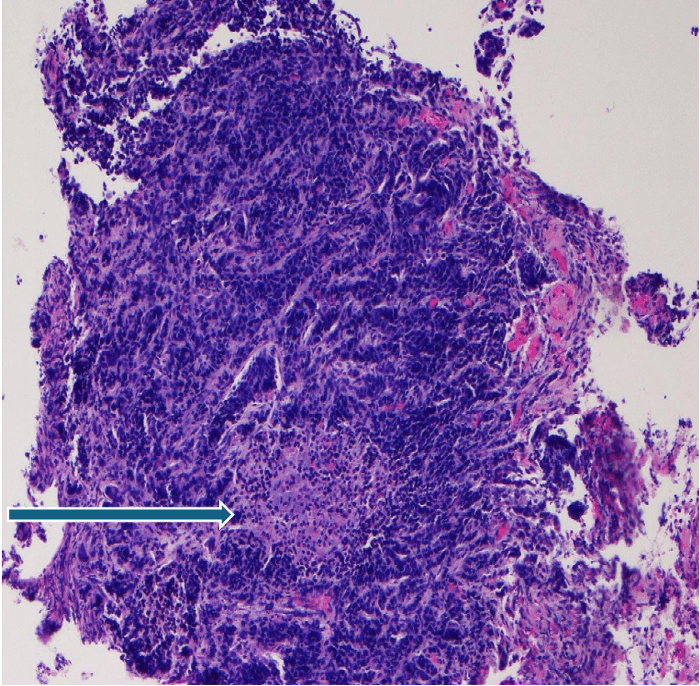
A 71-year-old woman with atrial fibrillation, heart failure with reduced ejection fraction, coronary artery disease, diabetes, and hypothyroidism presented with dyspnea, palpitations, and edema. Blood workup showed (hemoglobin 11.6 g/dL), and the Iron panel showed iron deficiency anemia (ferritin 48 ng/mL, TIBC 410 µg/dL). Non-contrast abdominal CT (Computed Tomography) revealed a 3.8 × 4.5 cm mass in the transverse colon with regional lymphadenopathy and a sub-centimeter omental nodule. Colonoscopy was performed and revealed a large, fungating, partially obstructing lesion 65 cm from the anal verge. Biopsies confirmed poorly differentiated medullary carcinoma. Due to cardiovascular instability, the need for ongoing anticoagulation, and malnutrition, surgery was deferred. Oncology was consulted and recommended outpatient Imaging and molecular profiling to guide systemic treatment.
Discussion:
Medullary carcinoma is a rare but distinct entity in colorectal cancer, often associated with microsatellite instability-high (MSI-H) status, which confers a better prognosis and eligibility for immunotherapy. While most cases are localized to the right colon, our case demonstrates that medullary features may present in less typical locations, such as the transverse colon. Diagnosis is often incidental and requires timely histologic confirmation and molecular testing. For patients who are not candidates for surgery, systemic therapy, particularly checkpoint inhibitors, plays a central role. Current National Comprehensive Cancer Network (NCCN) guidelines recommend pembrolizumab or nivolumab (± ipilimumab) as first-line options for MSI-H metastatic tumors. In this patient, comorbidities and functional status dictated a nonoperative approach, with a focus on individualized therapy based on tumor biology. Coordination between cardiology, oncology, and gastroenterology was essential to balancing risk and benefit in a medically complex scenario. Early diagnosis and molecular profiling are crucial for guiding personalized treatment, particularly in patients unable to undergo surgery.
Disclosures:
Sunny Kumar, MD1, Satish Kumar Ahuja, MD1, Rahul Kumar, MD2, Deepak Kumar, MBBS, MD3, Muhammad Sohaib Alvi, MBBS, MD4, Danial Nadeem, MD5, Joshua Charles Obuch, MD5, Renee Frank, MD6. P0338 - Medullary Carcinoma of the Transverse Colon in a Medically Complex Elderly Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
