Sunday Poster Session
Category: Colon
P0420 - Rapidly Progressing Rectal Neuroendocrine Tumor With Early Liver Metastasis Following Normal Screening
.jpeg.jpg)
Anudeep Jala, DO
Jefferson Health
Voorhees, NJ
Presenting Author(s)
1Jefferson Health, Voorhees, NJ; 2Jefferson Health, Somerdale, NJ; 3Jefferson Health, Blackwood, NJ; 4Jefferson Health, Stratford, NJ; 5Jefferson Health, Cherry Hill, NJ; 6Jefferson Health, Sewell, NJ
Introduction:
Rectal neuroendocrine tumors (NETs) are an uncommon type of cancer, accounting for about 1-2% of all rectal malignancies. Their incidence, however, has been rising in recent years. Rectal NETs exhibit a broad spectrum of behavior, ranging from indolent, well differentiated tumors to aggressive, poorly differentiated forms. Clinical presentations are equally variable, with patients experiencing symptoms such as abdominal pain, weight loss, anemia, or remaining entirely asymptomatic. We present a unique case of a rapidly progressing rectal neuroendocrine tumor following a normal screening colonoscopy.
Case Description/Methods:
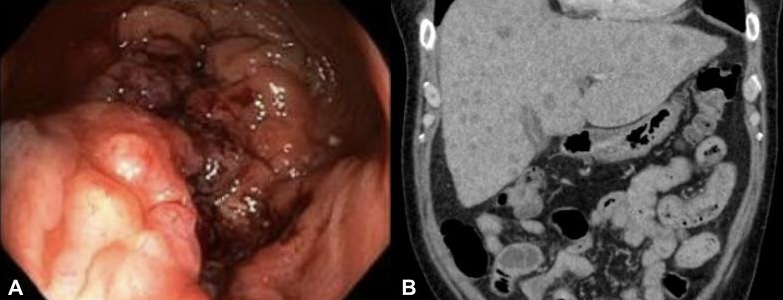
A 65-year-old male with a past medical history of diabetes, hypertension, and gastroesophageal reflux initially presented to the hospital for concern of right upper quadrant pain and jaundice. Labs notable for total bilirubin 6.8 mg/dL, direct bilirubin 4.2 mg/dL, alkaline phosphatase 258 IU/L, aspartate transferase (AST) 156 IU/L, and alanine aminotransferase (ALT) 167 IU/L. Of note, the patient had recently undergone a colonoscopy a few days prior to presentation for rectal pain and straining with bowel movements. Colonoscopy had noted an infiltrative, ulcerated mass in the distal rectum and biopsies were taken. Importantly, the patient had undergone a screening colonoscopy a year prior which was normal. Computed tomography (CT) scan with intravenous contrast of the abdomen was negative for any biliary obstruction but did demonstrate multiple hypodensities within the liver concerning for metastatic disease. Immunohistochemical staining was positive for CDX2, CK20, and SATB2, consistent with a diagnosis of poorly differentiated neuroendocrine carcinoma. The patient was eventually started with an inpatient chemotherapy regimen of carboplatin and etoposide.
Discussion:
This case highlights the aggressive nature and rapid progression of rectal neuroendocrine tumors, especially poorly differentiated subtypes. Despite a previously normal colonoscopy one year prior, the patient was found to have an advanced, infiltrative rectal mass with early metastatic spread to the liver. This emphasizes the variable nature of NETs, with some remaining indolent while others demonstrate rapid progression. Early detection remains a challenge as recent negative screening cannot fully exclude the possibility of rapidly progressive malignancies. Clinicians should maintain a high index of suspicion in patients with new onset gastrointestinal symptoms even in the setting of recent prior endoscopies.
Disclosures:
Anudeep Jala, DO1, Daniel Moodey, DO2, Sachin Prasad, DO3, Jason John, DO4, Seth Lipshutz, DO5, Marisa Pope, DO5, Edward Bley, DO6, Brian Blair, DO, FACG5. P0420 - Rapidly Progressing Rectal Neuroendocrine Tumor With Early Liver Metastasis Following Normal Screening, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
