Sunday Poster Session
Category: Colon
P0427 - Stercoral Perforation: Impact of Social Determinants of Health in a Case of Severe Opioid-Induced Constipation
Nasrin Sultana, MD
Harlem Hospital Center
New York, NY
Presenting Author(s)
1Harlem Hospital Center, New York, NY; 2NYC Health + Hospitals/Harlem, New York, NY; 3NYC Health + Hospitals, New York, NY
Introduction:
Stercoral perforation is a rare surgical emergency. Fecal impaction from chronic constipation can exert colonic wall pressure leading to necrosis, ulceration, and perforation. Incidence is 3.2% of all colonic perforations. Mortality is 34% due to delayed diagnosis and sepsis. Opioid-induced constipation (OIC) is a rarely reported risk factor. We present a case of a middle-aged man with opioid use disorder on methadone maintenance, who developed acute spontaneous sigmoid colon perforation in the context of untreated severe OIC.
Case Description/Methods:
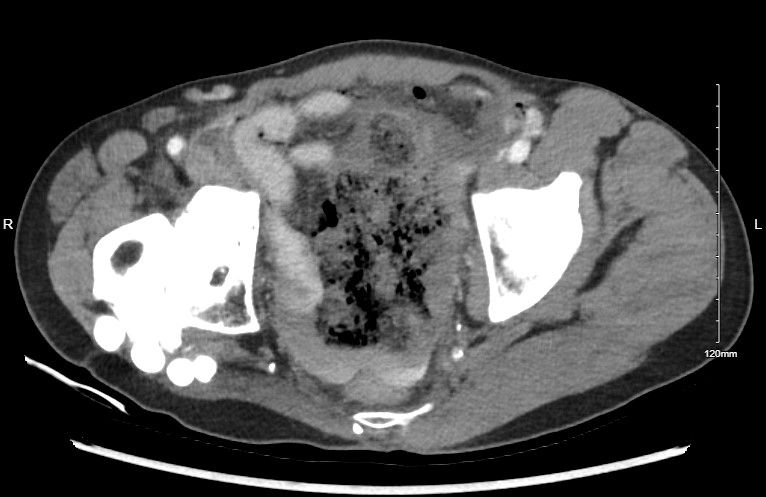
A 58-year-old male shelter resident with Hepatitis C, active intravenous heroin use, on methadone 160 mg daily, recent right hip surgery for osteomyelitis, and chronic malnutrition presented to the ED with severe generalized abdominal pain. He had three episodes of non-bloody non-bilious vomiting and dyspnea. He had not received his methadone dose that day. He appeared ill and cachectic. He was hypotensive (BP 64/81 mmHg), tachycardic (HR 115 bpm), with a rigid abdomen. He had leukopenia (WBC 1.84 ×10³/μL), hyperkalemia (K⁺ 7.2 mmol/L), metabolic acidosis (lactate 6.1 mmol/L) and hyperglycemia (238 mg/dL). CT abdomen revealed a perforated proximal sigmoid colon, extraluminal fecal material, and large-volume pneumoperitoneum raising concern for fecal peritonitis ( Figure 1, Figure 2). Emergent exploratory laparotomy revealed a sigmoid colon perforation with fecal contamination. A partial sigmoidectomy without primary anastomosis was performed, followed by abdominal washout and wound VAC placement. Post-operatively, he developed septic shock and was treated with multiple broad-spectrum antibiotics.
Discussion:
Patients requiring therapy with long-acting opioids, like methadone, are at increased risk of OIC. This risk may be compounded by continued use of short-acting opiates like heroin. Our patient had severe untreated OIC. Peripherally acting mu opiate receptor antagonists can ameliorate symptoms by reversing motility effects at the gut level without inhibiting the CNS effects. Beyond the physiological mechanisms, social determinants of health play a critical role in the trajectory of such conditions. Homelessness, limited healthcare access, substance use, malnutrition, and health illiteracy can significantly delay management and worsen outcomes. Our patient was homeless with active opioid use disorder, had malnutrition, and poor health literacy. Addressing those social determinants of health may prevent such grave complications.

Disclosures:
Nasrin Sultana, MD1, FNU Allahyar, MD1, Esteban Verduzco, MD, MMSc2, Mohamed K.. Osman, MD, MPH2, Joan A.. Culpepper-Morgan, MD, FACG3. P0427 - Stercoral Perforation: Impact of Social Determinants of Health in a Case of Severe Opioid-Induced Constipation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
