Sunday Poster Session
Category: Diet, Nutrition, and Obesity
P0571 - Impact of Protein-Calorie Malnutrition on Outcomes in Clostridioides difficile Infection: A Propensity-Matched Analysis Using TriNetX
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ashujot K. Dang, MD
University of California Riverside School of Medicine
Riverside, CA
Presenting Author(s)
Ashujot K. Dang, MD1, Shivam Kalra, MBBS, MHA2, Angad Mann, MD3, Amaninder Dhaliwal, MD4, Paul Leonor, MD5
1University of California Riverside School of Medicine, Riverside, CA; 2Trident Medical Center, North Charleston, SC; 3University of California Riverside School of Medicine, Rancho Cucamonga, CA; 4University of South Carolina School of Medicine, Florence, SC; 5Loma Linda University Medical Center, Loma Linda, CA
Introduction: Clostridium difficile infection (CDI), a known nosocomial infection, increases the mortality rates by 2.4 times. The most affected group is patients with protein-calorie malnutrition (PCM), which is highly prevalent in hospitalized patients with chronic illness, advanced age, and prolonged stay. PCM and CDI are pathophysiologically linked. PCM alters the gut biome, which increases susceptibility to CDI. CDI further exaggerates malnutrition through diarrhea. We aim to study the magnitude of impact of PCM on CDI and form preventative strategies to improve overall patient outcomes.
Methods: A retrospective cohort study was conducted using the TriNetX US Collaborative Network. Adults with CDI were divided into two cohorts based on the presence (PCM+) or absence (PCM−) of concurrent PCM. Propensity score matching (1:1) was performed across 103,052 patients per group. The primary outcome was 30-day mortality. Secondary outcomes included sepsis, septic shock, toxic megacolon, colectomy, ileus, intestinal perforation, ischemic colitis, abdominal abscess, acute kidney injury (AKI), and 30-day readmission. Hazard ratios (HR) and 95% confidence intervals (CI) were calculated using Kaplan-Meier survival analyses.
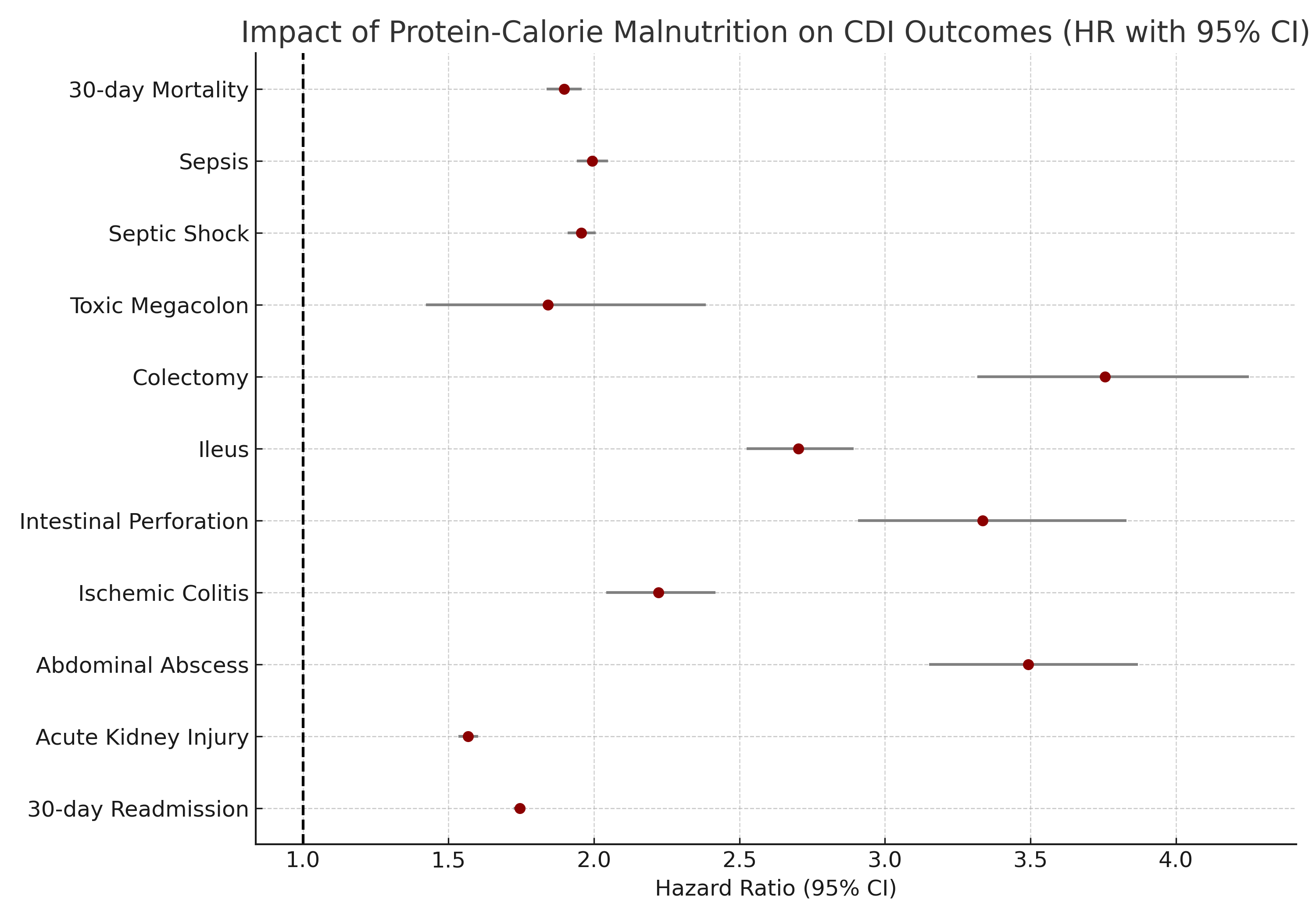
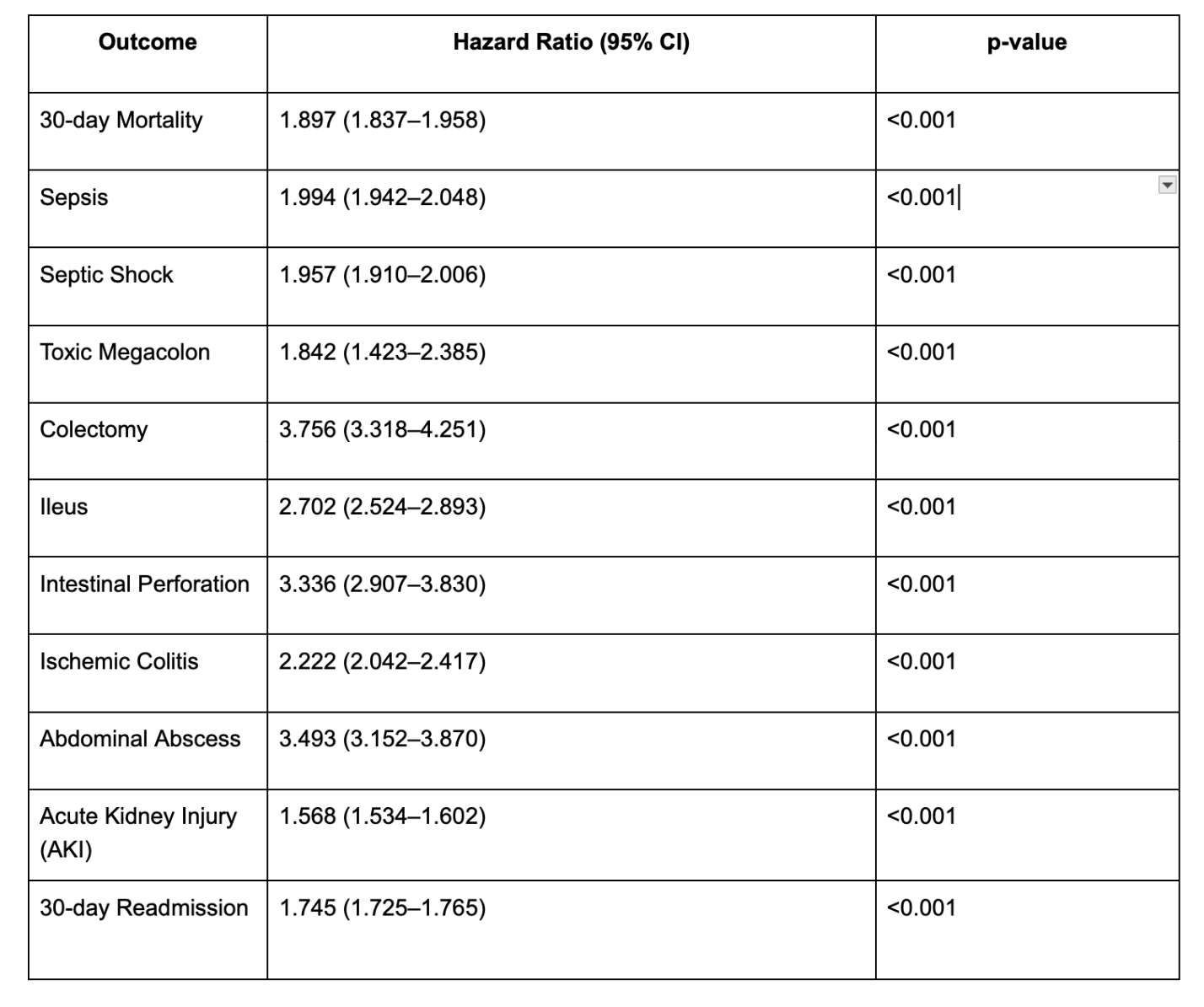
Results: Compared to PCM− patients, those with PCM+ had significantly worse outcomes. PCM was associated with higher 30-day mortality (HR 1.897, 95% CI 1.837–1.958), sepsis (HR 1.994), septic shock (HR 1.957), and colectomy (HR 3.756). Additional elevated risks were seen for ileus (HR 2.702), intestinal perforation (HR 3.336), ischemic colitis (HR 2.222), abdominal abscess (HR 3.493), AKI (HR 1.568), and 30-day readmission (HR 1.745), all p< 0.001.
Discussion: As evident by the result above, malnutrition has a direct impact on CDI with increased mortality and complications such as sepsis, toxic megacolon, and prolonged hospitalization. Hence, early identification and correction of PCM are critical in patients with CDI. Nutritional assessment should be performed promptly, and nutritional support (preferably enteral, if feasible) should be initiated early to prevent ADRs. Albumin is an acute-phase reactant and is known to fluctuate with inflammation, hence, there is a need for standardized definitions of malnutrition and further clinical trials on the role of diet and non-pharmacologic interventions in CDI.
Disclosures:
Ashujot K. Dang, MD1, Shivam Kalra, MBBS, MHA2, Angad Mann, MD3, Amaninder Dhaliwal, MD4, Paul Leonor, MD5. P0571 - Impact of Protein-Calorie Malnutrition on Outcomes in <i>Clostridioides difficile</i> Infection: A Propensity-Matched Analysis Using TriNetX, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Riverside School of Medicine, Riverside, CA; 2Trident Medical Center, North Charleston, SC; 3University of California Riverside School of Medicine, Rancho Cucamonga, CA; 4University of South Carolina School of Medicine, Florence, SC; 5Loma Linda University Medical Center, Loma Linda, CA
Introduction: Clostridium difficile infection (CDI), a known nosocomial infection, increases the mortality rates by 2.4 times. The most affected group is patients with protein-calorie malnutrition (PCM), which is highly prevalent in hospitalized patients with chronic illness, advanced age, and prolonged stay. PCM and CDI are pathophysiologically linked. PCM alters the gut biome, which increases susceptibility to CDI. CDI further exaggerates malnutrition through diarrhea. We aim to study the magnitude of impact of PCM on CDI and form preventative strategies to improve overall patient outcomes.
Methods: A retrospective cohort study was conducted using the TriNetX US Collaborative Network. Adults with CDI were divided into two cohorts based on the presence (PCM+) or absence (PCM−) of concurrent PCM. Propensity score matching (1:1) was performed across 103,052 patients per group. The primary outcome was 30-day mortality. Secondary outcomes included sepsis, septic shock, toxic megacolon, colectomy, ileus, intestinal perforation, ischemic colitis, abdominal abscess, acute kidney injury (AKI), and 30-day readmission. Hazard ratios (HR) and 95% confidence intervals (CI) were calculated using Kaplan-Meier survival analyses.
Results: Compared to PCM− patients, those with PCM+ had significantly worse outcomes. PCM was associated with higher 30-day mortality (HR 1.897, 95% CI 1.837–1.958), sepsis (HR 1.994), septic shock (HR 1.957), and colectomy (HR 3.756). Additional elevated risks were seen for ileus (HR 2.702), intestinal perforation (HR 3.336), ischemic colitis (HR 2.222), abdominal abscess (HR 3.493), AKI (HR 1.568), and 30-day readmission (HR 1.745), all p< 0.001.
Discussion: As evident by the result above, malnutrition has a direct impact on CDI with increased mortality and complications such as sepsis, toxic megacolon, and prolonged hospitalization. Hence, early identification and correction of PCM are critical in patients with CDI. Nutritional assessment should be performed promptly, and nutritional support (preferably enteral, if feasible) should be initiated early to prevent ADRs. Albumin is an acute-phase reactant and is known to fluctuate with inflammation, hence, there is a need for standardized definitions of malnutrition and further clinical trials on the role of diet and non-pharmacologic interventions in CDI.
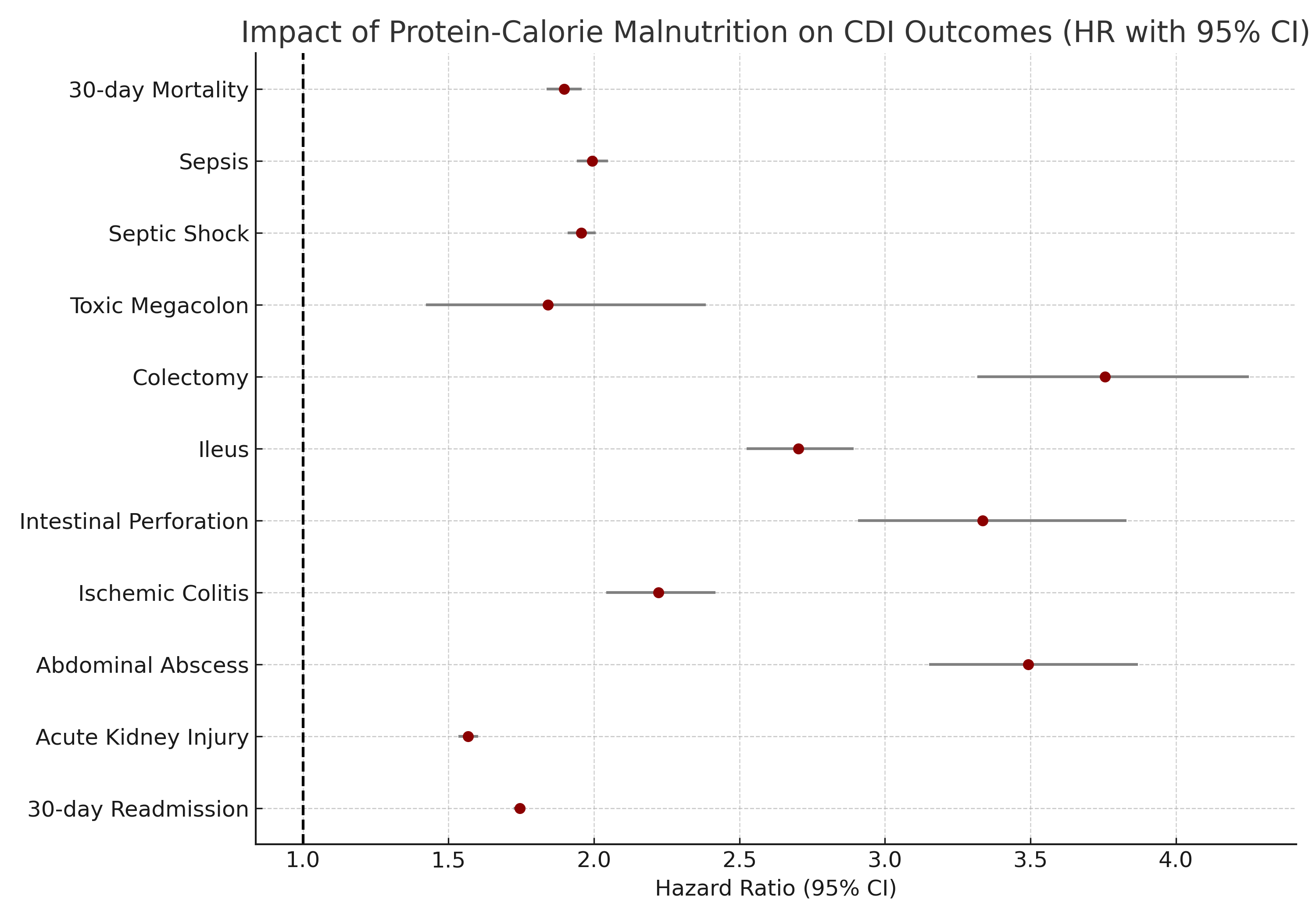
Figure: Hazard ratios depicting the impact of PCM on CDI outcomes
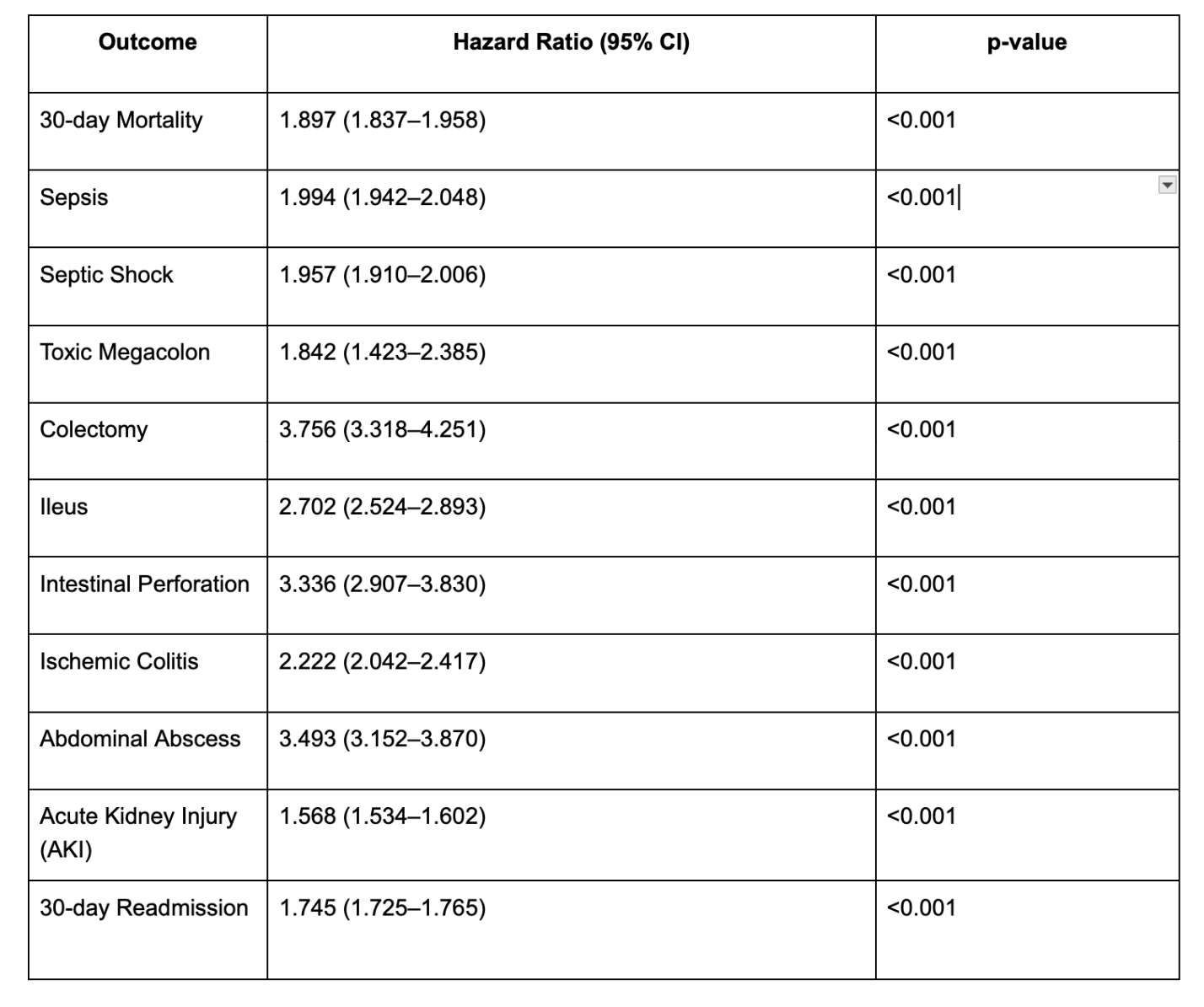
Figure: Table depicting the outcomes with confidence intervals and p-values for each CDI outcome.
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Shivam Kalra indicated no relevant financial relationships.
Angad Mann indicated no relevant financial relationships.
Amaninder Dhaliwal indicated no relevant financial relationships.
Paul Leonor indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Shivam Kalra, MBBS, MHA2, Angad Mann, MD3, Amaninder Dhaliwal, MD4, Paul Leonor, MD5. P0571 - Impact of Protein-Calorie Malnutrition on Outcomes in <i>Clostridioides difficile</i> Infection: A Propensity-Matched Analysis Using TriNetX, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
