Sunday Poster Session
Category: Endoscopy Video Forum
P0591 - Endoscopic Reconstruction of Symptomatic Pre-Stenotic Gastric Sleeve Dilation

Harsimran Kalsi, MD
University of Central Florida
Gainesville, FL
Presenting Author(s)
1University of Central Florida, Gainesville, FL; 2Mount Sinai South Nassau,Icahn School of Medicine at Mount Sinai, Oceanside, NY; 3Cedars-Sinai Medical Center, Santa Monica, CA
Introduction:
Anatomical remodeling and gastric sleeve dysmotility of a gastric sleeve due to chronic downstream gastric stenosis is an underrecognized sequence of complications following laparoscopic sleeve gastrectomy (LSG). Patients may present with persistent nausea, vomiting, and oral intolerance in spite of successful treatment of gastric sleeve stenosis due to retention of gastric contents in the proximal sleeve. We present a case of endoscopic reconstruction of symptomatic pre-stenotic gastric sleeve dilation.
Case Description/Methods:
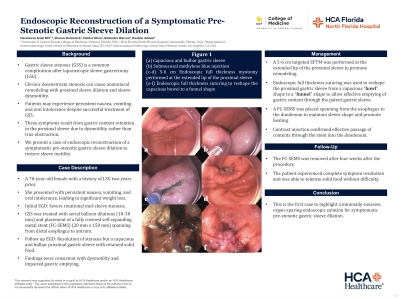
A 70-year-old female with a history of LSG two years prior presented with persistent nausea, vomiting, and oral intolerance, resulting in significant unintended weight loss.
Prior Interventions
Initial esophagogastroduodenoscopy (EGD) revealed a severe rotational sleeve stenosis in the mid-body of the gastric sleeve. Over several months, she underwent serial endoscopic balloon dilations (from 18 mm to 30 mm) and placement of a fully covered self-expanding metal stent (20 mm × 150 mm), spanning from the distal esophagus to the antrum. While the stenosis was successfully treated, the patient continued to experience postprandial emesis with only partial symptom relief.
Successful Management
Surveillance EGD showed resolution of the mid-sleeve stenosis with unobstructed contrast flow. However, a markedly capacious and bulbar proximal gastric sleeve with retained solid food was noted, consistent with impaired motility rather than mechanical obstruction. A 5-6 cm targeted full-thickness myotomy was performed at the extended lip of the proximal sleeve to promote remodeling. Endoscopic full-thickness suturing was used to reshape the proximal gastric sleeve from a capacious “bowl” shape to a “funnel” shape to allow effective emptying of gastric content through the patent gastric sleeve. A fully covered esophageal stent was placed from the esophagus to the duodenum to promote tissue healing in the desired configuration. Contrast injection confirmed effective passage of contents through the stent into the duodenum.
Follow-Up
The stent was removed after four weeks. Following the procedure, the patient experienced complete symptom resolution and was able to tolerate solid foods without difficulty.
Discussion: This is the first case to highlight a minimally-invasive, organ-sparing endoscopic approach in the treatment of symptomatic pre-stenotic gastric sleeve dilation through EFTM, endoscopic suturing, and stenting.
Disclosures:
Harsimran Kalsi, MD1, Sharon Slomovich, MD2, Haidar Khan, MD2, Rabindra Watson, MD3, Rashmi Advani, MD2. P0591 - Endoscopic Reconstruction of Symptomatic Pre-Stenotic Gastric Sleeve Dilation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
