Sunday Poster Session
Category: Functional Bowel Disease
P0789 - Overlooked and Undertreated: National Shortfalls in Anorectal Evaluation for Gastroparesis-Associated Constipation
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohamed Eldesouki, MD
Saint Michael's Medical Center, New York Medical College
Newark, NJ
Presenting Author(s)
Mohamed Eldesouki, MD1, Ahmed Ibrahim, MD2, Ahmed Salem, MD3, Mohammad Kloub, MD4, Hazem Abosheaishaa, MD5, Amol Sharma, MD, MSc, FACG2
1Saint Michael's Medical Center, New York Medical College, Newark, NJ; 2Medical University of South Carolina, Charleston, SC; 3Maimonides Medical Center, Brooklyn, NY; 4New York Medical College - Saint Michael's Medical Center, Bloomfield, NJ; 5Mount Sinai West, Icahn School of Medicine at Mount Sinai, Queens, NY
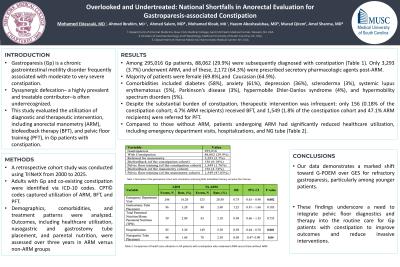
Introduction: Gastroparesis (Gp) is a chronic gastrointestinal motility disorder frequently associated with moderate to very severe constipation. Dyssynergic defecation– a highly prevalent and treatable contributor–is often underrecognized. This study evaluated the utilization of diagnostic and therapeutic intervention, including anorectal manometry (ARM), biofeedback therapy (BFT), and pelvic floor training (PFT), in Gp patients with constipation.
Methods: A retrospective cohort study was conducted using TriNetX from 2000 to 2025. Adults with Gp and co-existing constipation were identified via ICD-10 codes. CPT© codes captured utilization of ARM, BFT, and PFT. Demographics, comorbidities, and treatment patterns were analyzed. Outcomes, including healthcare utilization, nasogastric and gastrostomy tube placement, and parental nutrition, were assessed over three years in ARM versus non-ARM groups.
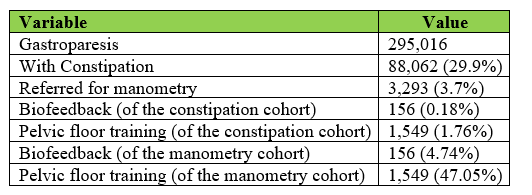
Results: Among 295,016 Gp patients, 88,062 (29.9%) were subsequently diagnosed with constipation (Table 1). Only 3,293 (3.7%) underwent ARM, and of these, 2,172 (64.3%) were prescribed secretory pharmacologic agents post-ARM. Gp patients with constipation undergoing ARM were predominantly female (69.8%), Caucasian (64.9%), with African American (18.6%) and Hispanic (8.7%) representation. Comorbidities included diabetes (58%), anxiety (61%), depression (36%), scleroderma (3%), systemic lupus erythematosus (5%), Parkinson’s disease (3%), hypermobile Ehler-Danlos syndrome (4%), and hypermobility spectrum disorders (5%).
Despite the substantial burden of constipation, therapeutic intervention was infrequent: only 156 (0.18% of the constipation cohort; 4.7% ARM recipients) received BFT, and 1,549 (1.8% of the constipation cohort and 47.1% ARM recipients) were referred for PFT. Among those receiving BFT or PFT, 90.8% were female, 73% Caucasian, 17.6% African American, and 7% Hispanic, with most aged 25–45 years.
Compared to those without ARM, patients undergoing ARM had significantly reduced healthcare utilization, including emergency department visits, hospitalizations, and NG tube (Table 2).
Discussion: This large national cohort highlights the striking underutilization of ARM, BFT, and PFG in Gp patients with constipation, despite guideline-based support for anorectal evaluation and therapy in constipation. These findings underscore a need to integrate pelvic floor diagnostics and therapy into the routine care for Gp patients with constipation to improve outcomes and reduce invasive interventions.
Disclosures:
Mohamed Eldesouki, MD1, Ahmed Ibrahim, MD2, Ahmed Salem, MD3, Mohammad Kloub, MD4, Hazem Abosheaishaa, MD5, Amol Sharma, MD, MSc, FACG2. P0789 - Overlooked and Undertreated: National Shortfalls in Anorectal Evaluation for Gastroparesis-Associated Constipation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Saint Michael's Medical Center, New York Medical College, Newark, NJ; 2Medical University of South Carolina, Charleston, SC; 3Maimonides Medical Center, Brooklyn, NY; 4New York Medical College - Saint Michael's Medical Center, Bloomfield, NJ; 5Mount Sinai West, Icahn School of Medicine at Mount Sinai, Queens, NY
Introduction: Gastroparesis (Gp) is a chronic gastrointestinal motility disorder frequently associated with moderate to very severe constipation. Dyssynergic defecation– a highly prevalent and treatable contributor–is often underrecognized. This study evaluated the utilization of diagnostic and therapeutic intervention, including anorectal manometry (ARM), biofeedback therapy (BFT), and pelvic floor training (PFT), in Gp patients with constipation.
Methods: A retrospective cohort study was conducted using TriNetX from 2000 to 2025. Adults with Gp and co-existing constipation were identified via ICD-10 codes. CPT© codes captured utilization of ARM, BFT, and PFT. Demographics, comorbidities, and treatment patterns were analyzed. Outcomes, including healthcare utilization, nasogastric and gastrostomy tube placement, and parental nutrition, were assessed over three years in ARM versus non-ARM groups.
Results: Among 295,016 Gp patients, 88,062 (29.9%) were subsequently diagnosed with constipation (Table 1). Only 3,293 (3.7%) underwent ARM, and of these, 2,172 (64.3%) were prescribed secretory pharmacologic agents post-ARM. Gp patients with constipation undergoing ARM were predominantly female (69.8%), Caucasian (64.9%), with African American (18.6%) and Hispanic (8.7%) representation. Comorbidities included diabetes (58%), anxiety (61%), depression (36%), scleroderma (3%), systemic lupus erythematosus (5%), Parkinson’s disease (3%), hypermobile Ehler-Danlos syndrome (4%), and hypermobility spectrum disorders (5%).
Despite the substantial burden of constipation, therapeutic intervention was infrequent: only 156 (0.18% of the constipation cohort; 4.7% ARM recipients) received BFT, and 1,549 (1.8% of the constipation cohort and 47.1% ARM recipients) were referred for PFT. Among those receiving BFT or PFT, 90.8% were female, 73% Caucasian, 17.6% African American, and 7% Hispanic, with most aged 25–45 years.
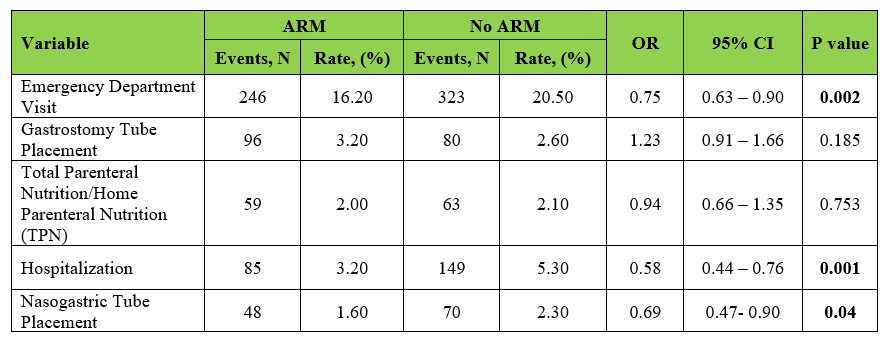
Compared to those without ARM, patients undergoing ARM had significantly reduced healthcare utilization, including emergency department visits, hospitalizations, and NG tube (Table 2).
Discussion: This large national cohort highlights the striking underutilization of ARM, BFT, and PFG in Gp patients with constipation, despite guideline-based support for anorectal evaluation and therapy in constipation. These findings underscore a need to integrate pelvic floor diagnostics and therapy into the routine care for Gp patients with constipation to improve outcomes and reduce invasive interventions.
Figure: Table 1: Description of the Gastroparesis Cohort with constipation undergoing anorectal manometry, biofeedback therapy, and pelvic floor physical therapy.
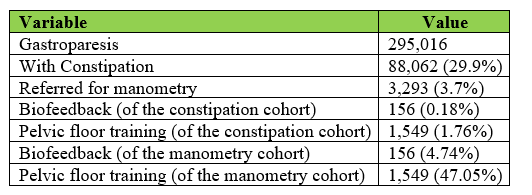
Figure: Table 2: Comparison of Healthcare Utilization in Gp patients with constipation who underwent ARM versus those without ARM.
Disclosures:
Mohamed Eldesouki indicated no relevant financial relationships.
Ahmed Ibrahim indicated no relevant financial relationships.
Ahmed Salem indicated no relevant financial relationships.
Mohammad Kloub indicated no relevant financial relationships.
Hazem Abosheaishaa indicated no relevant financial relationships.
Amol Sharma indicated no relevant financial relationships.
Mohamed Eldesouki, MD1, Ahmed Ibrahim, MD2, Ahmed Salem, MD3, Mohammad Kloub, MD4, Hazem Abosheaishaa, MD5, Amol Sharma, MD, MSc, FACG2. P0789 - Overlooked and Undertreated: National Shortfalls in Anorectal Evaluation for Gastroparesis-Associated Constipation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
