Sunday Poster Session
Category: Functional Bowel Disease
P0818 - Disparities in Prophylactic Medication Use for Cyclic Vomiting Syndrome Between Academic and Non-academic Hospitals: A Retrospective Cohort Study Using the TriNetX Network
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Has Audio

Saranya Arumugam, MD
University of California Riverside School of Medicine
Riverside, CA
Presenting Author(s)
Saranya Arumugam, MD1, Muhammad Ayyan, MBBS2, Mahima Vyas, MBBS2, Ashujot K. Dang, MD1, Thangam Venkatesan, MD2
1University of California Riverside School of Medicine, Riverside, CA; 2The Ohio State University, Columbus, OH
Introduction: Cyclic Vomiting Syndrome (CVS) is a debilitating disorder of gut-brain interaction, characterized by recurrent episodes of nausea and vomiting. The American Neurogastroenterology and Motility Society (ANMS) recommends prophylactic therapy such as tricyclic antidepressants, topiramate or aprepitant for moderate-to-severe CVS. Despite this, many patients do not receive the recommended therapy, potentially contributing to increased healthcare burden and poor outcomes. This study aimed to evaluate the prescription rates of guideline-recommended prophylactic medications in patients with CVS in both academic and non-academic centers.
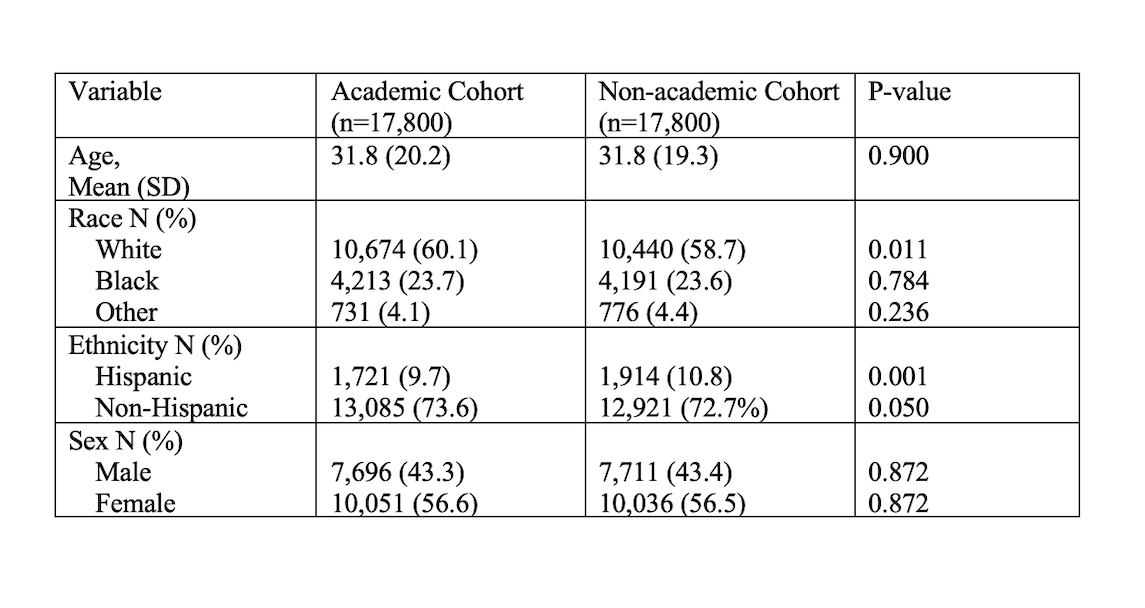
Methods: A retrospective cohort study comparing rates of prophylactic medication use in CVS patients between academic and non-academic centers was performed using TriNetX, a multicentre electronic health record database. Those with depression, bipolar disorder, epilepsy, recurrent seizures, malignancy, or receiving chemotherapy or immunotherapy were excluded as they may have been prescribed these medications for other indications. Cohorts were matched for age, race, and ethnicity. After matching, each group included 17,800 patients.
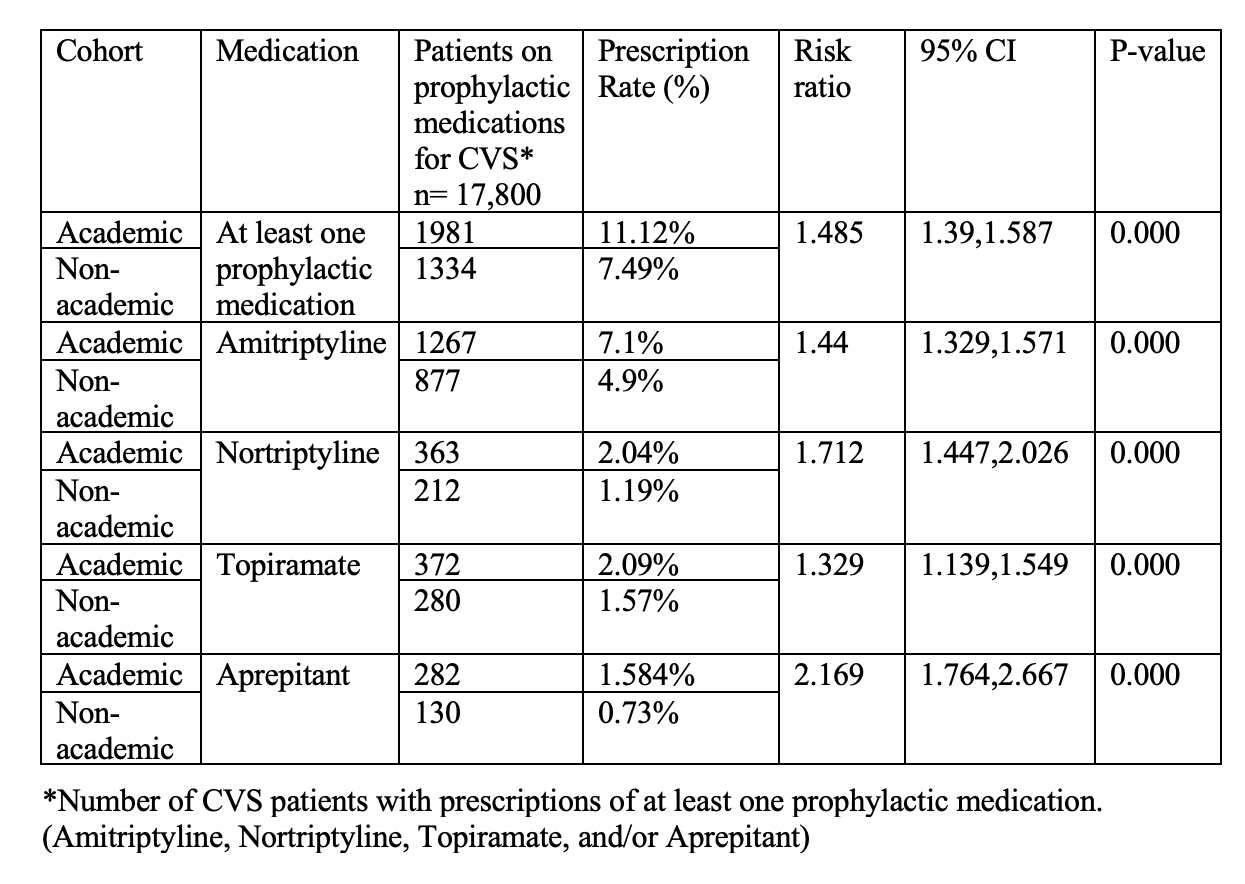
Results: Baseline characteristics of patients is shown in Table 1. Prescription rates for CVS prophylaxis were significantly higher in academic settings vs non-academic settings [11.1% vs 7.49%, p value = < 0.0001] with a RR 1.48; 95% CI: 1.39-1.587. Amitriptyline was the most commonly prescribed agent, followed by nortriptyline, topiramate and aprepitant (Table 2). Aprepitant had the lowest prescription rates overall, with 282 patients (1.5%) in academic centres and 130 patients (0.73%) in non-academic centres (RR = 2.2).
Discussion: Guideline-directed pharmacologic prophylaxis for CVS is low, with notable disparities between academic and non-academic centres. Limitations include reliance on diagnostic coding and the retrospective nature of the study. Nonetheless, our study, using a large national database, shows poor adherence to guidelines for CVS management in the medical community. Reasons for these are unclear but might be due to physicians being uncomfortable using neuromodulators and gaps in training in Neurogastroenterology. These findings underscore the need for targeted strategies, including clinician education and referral to specialized CVS centres to enhance CVS care delivery and outcomes.
Disclosures:
Saranya Arumugam, MD1, Muhammad Ayyan, MBBS2, Mahima Vyas, MBBS2, Ashujot K. Dang, MD1, Thangam Venkatesan, MD2. P0818 - POSTER WITHDRAWN, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Riverside School of Medicine, Riverside, CA; 2The Ohio State University, Columbus, OH
Introduction: Cyclic Vomiting Syndrome (CVS) is a debilitating disorder of gut-brain interaction, characterized by recurrent episodes of nausea and vomiting. The American Neurogastroenterology and Motility Society (ANMS) recommends prophylactic therapy such as tricyclic antidepressants, topiramate or aprepitant for moderate-to-severe CVS. Despite this, many patients do not receive the recommended therapy, potentially contributing to increased healthcare burden and poor outcomes. This study aimed to evaluate the prescription rates of guideline-recommended prophylactic medications in patients with CVS in both academic and non-academic centers.
Methods: A retrospective cohort study comparing rates of prophylactic medication use in CVS patients between academic and non-academic centers was performed using TriNetX, a multicentre electronic health record database. Those with depression, bipolar disorder, epilepsy, recurrent seizures, malignancy, or receiving chemotherapy or immunotherapy were excluded as they may have been prescribed these medications for other indications. Cohorts were matched for age, race, and ethnicity. After matching, each group included 17,800 patients.
Results: Baseline characteristics of patients is shown in Table 1. Prescription rates for CVS prophylaxis were significantly higher in academic settings vs non-academic settings [11.1% vs 7.49%, p value = < 0.0001] with a RR 1.48; 95% CI: 1.39-1.587. Amitriptyline was the most commonly prescribed agent, followed by nortriptyline, topiramate and aprepitant (Table 2). Aprepitant had the lowest prescription rates overall, with 282 patients (1.5%) in academic centres and 130 patients (0.73%) in non-academic centres (RR = 2.2).
Discussion: Guideline-directed pharmacologic prophylaxis for CVS is low, with notable disparities between academic and non-academic centres. Limitations include reliance on diagnostic coding and the retrospective nature of the study. Nonetheless, our study, using a large national database, shows poor adherence to guidelines for CVS management in the medical community. Reasons for these are unclear but might be due to physicians being uncomfortable using neuromodulators and gaps in training in Neurogastroenterology. These findings underscore the need for targeted strategies, including clinician education and referral to specialized CVS centres to enhance CVS care delivery and outcomes.
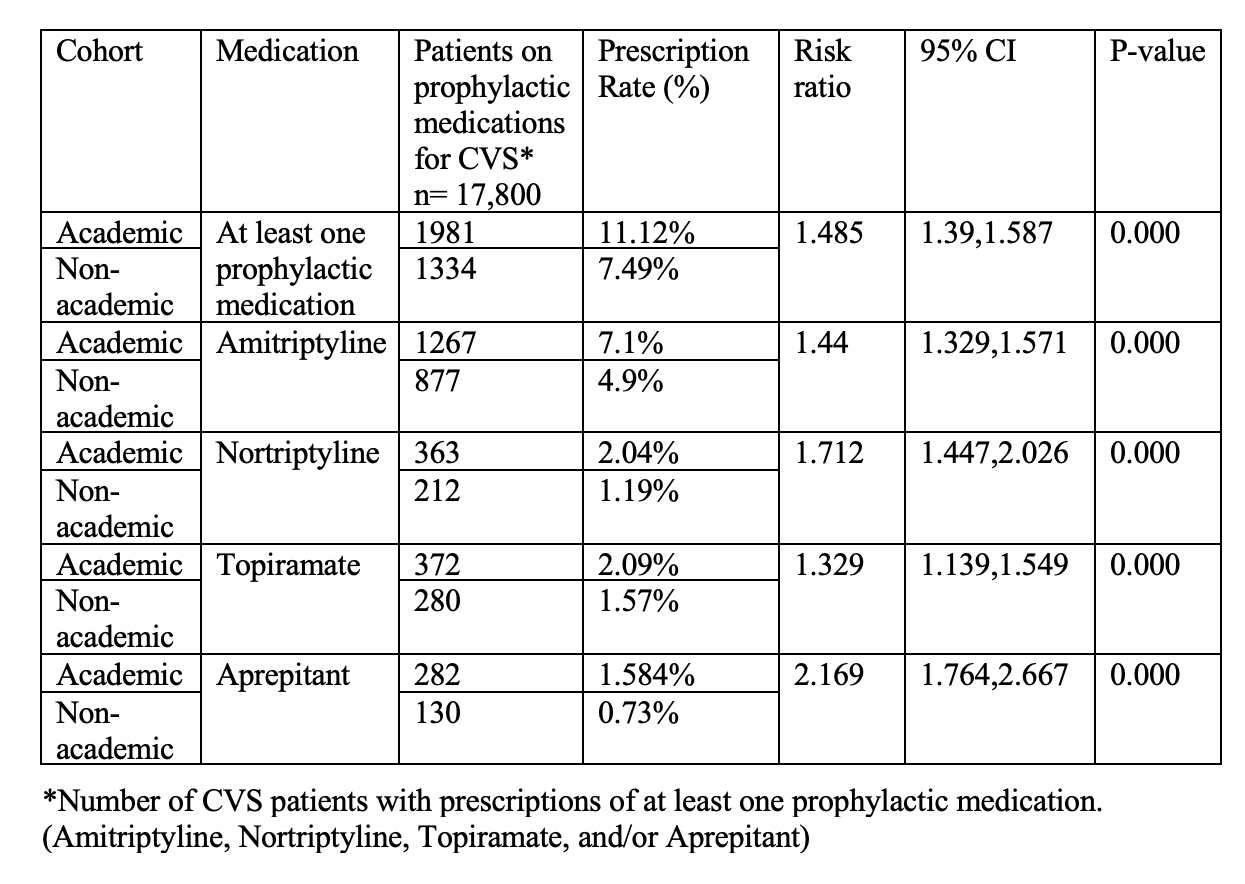
Figure: Table 1: Baseline Characteristics of CVS patients in Academic vs Non-Academic Center Cohorts
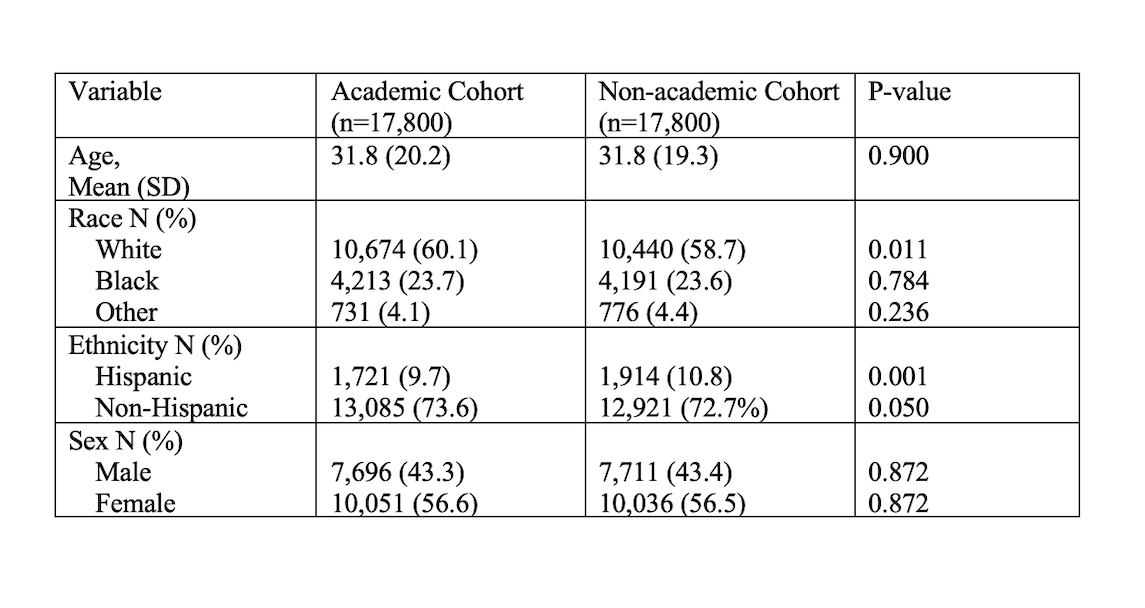
Figure: Table 2: Prescription Rates of Prophylactic Medications Among Matched CVS Patients in Academic vs. Non-Academic Centers
Disclosures:
Saranya Arumugam indicated no relevant financial relationships.
Muhammad Ayyan indicated no relevant financial relationships.
Mahima Vyas indicated no relevant financial relationships.
Ashujot Dang indicated no relevant financial relationships.
Thangam Venkatesan: Azurity – Consultant. Takeda Pharmaceuticals – Consultant, Grant/Research Support.
Saranya Arumugam, MD1, Muhammad Ayyan, MBBS2, Mahima Vyas, MBBS2, Ashujot K. Dang, MD1, Thangam Venkatesan, MD2. P0818 - POSTER WITHDRAWN, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

