Sunday Poster Session
Category: Functional Bowel Disease
P0819 - Cannabis Use Is Associated With an Increased Incidence of Gastroparesis and Cyclic Vomiting Syndrome but Not Inflammatory Bowel Disease in the US: A Multicentre Cohort Study Using the Trinetx Network
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Has Audio

Saranya Arumugam, MD
University of California Riverside School of Medicine
Riverside, CA
Presenting Author(s)
Saranya Arumugam, MD1, Omayma Alshaarawy, PhD2, Khaled Al Smadi, MD3, Thangam Venkatesan, MD4
1University of California Riverside School of Medicine, Riverside, CA; 2Michigan State University, East Lansing, MI; 3University of California Riverside, Riverside, CA; 4The Ohio State University, Columbus, OH
Introduction: Cannabis is used by patients for its anti-emetic properties, but paradoxically chronic use has been associated with vomiting disorders. Chronic cannabis use can downregulate cannabinoid receptors disrupting emesis homeostasis and reduce gastric motility. Understanding the effects of cannabis use is crucial given legalization, increased use of cannabis and public perception of safety in the United States. Therefore, we aimed to evaluate the incidence of cyclic vomiting syndrome (CVS) and gastroparesis (GP) among cannabis users versus non-users and compare these with inflammatory bowel disease (IBD), as a contrasting organic condition with distinct pathophysiology.
Methods: A retrospective cohort study was conducted using the TriNetX, a large multicenter electronic health record database to determine the incidence of GP, CVS and IBD in cannabis vs non-cannabis users. Cohort 1 included patients with documented cannabis use, while Cohort 2 (non-users) was constructed using vitamin D users (a required variable for cohort creation in TriNetX). Exclusion criteria included GI malignancies, pregnancy, chronic opioid use, use of GLP-1 agonists, organic gastrointestinal (GI) conditions and neurological conditions known to impact GI motility. Propensity score matching (1:1) was performed to balance both cohorts on key demographic and clinical variables, including age, gender, comorbidity index, BMI range, tobacco use, alcohol use, diabetes, and socioeconomic status. After matching, each cohort included 456,016 patients.
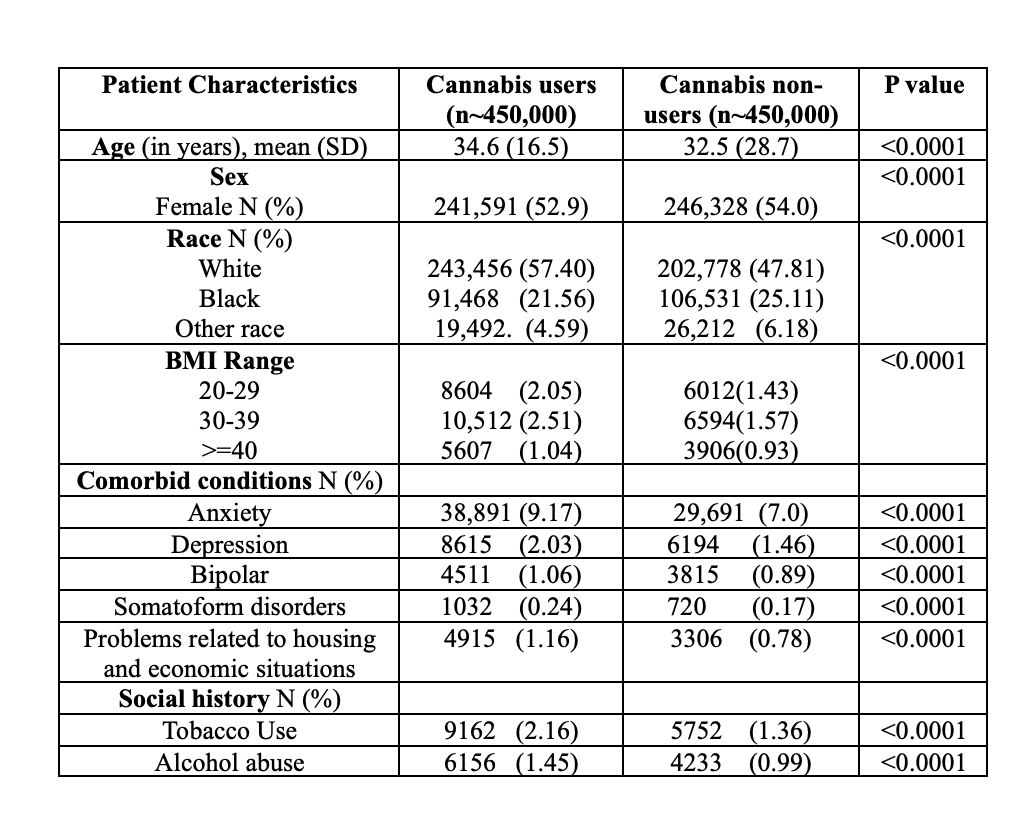
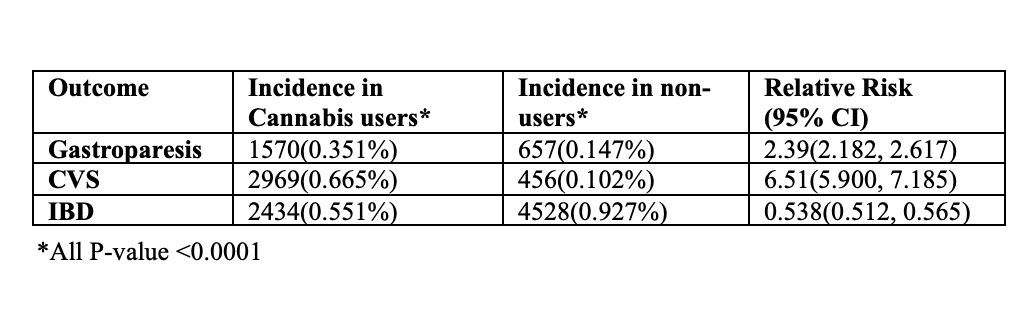
Results: Baseline demographic and clinical characteristics of the matched cohorts are summarized in Table 1. CVS was identified in 0.67% vs 0.10% [RR 6.5, CI (5.9, 7.19)], GP in 0.35% vs.0.15% [RR 2.399, CI (2.18, 2.62)] and IBD in 0.55% vs 0.93% [RR,0.538 CI (0.51, 0.57)] in cannabis users versus non-users respectively (all p < 0.001).
Discussion: This study demonstrates a significantly increased risk of CVS and GP among cannabis users compared to non-users in contrast to IBD which had a lower incidence. The directionality of these associations and whether cannabis causes or worsens vomiting or is used by CVS and GP patients due to a lack of targeted therapies is unclear. Limitations include the use of a database and retrospective coding. However, this is the largest study on this topic to our knowledge with ~ a million patients and further prospective research to better understand the effects of cannabis use on CVS and GP are warranted.
Disclosures:
Saranya Arumugam, MD1, Omayma Alshaarawy, PhD2, Khaled Al Smadi, MD3, Thangam Venkatesan, MD4. P0819 - POSTER WITHDRAWN, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Riverside School of Medicine, Riverside, CA; 2Michigan State University, East Lansing, MI; 3University of California Riverside, Riverside, CA; 4The Ohio State University, Columbus, OH
Introduction: Cannabis is used by patients for its anti-emetic properties, but paradoxically chronic use has been associated with vomiting disorders. Chronic cannabis use can downregulate cannabinoid receptors disrupting emesis homeostasis and reduce gastric motility. Understanding the effects of cannabis use is crucial given legalization, increased use of cannabis and public perception of safety in the United States. Therefore, we aimed to evaluate the incidence of cyclic vomiting syndrome (CVS) and gastroparesis (GP) among cannabis users versus non-users and compare these with inflammatory bowel disease (IBD), as a contrasting organic condition with distinct pathophysiology.
Methods: A retrospective cohort study was conducted using the TriNetX, a large multicenter electronic health record database to determine the incidence of GP, CVS and IBD in cannabis vs non-cannabis users. Cohort 1 included patients with documented cannabis use, while Cohort 2 (non-users) was constructed using vitamin D users (a required variable for cohort creation in TriNetX). Exclusion criteria included GI malignancies, pregnancy, chronic opioid use, use of GLP-1 agonists, organic gastrointestinal (GI) conditions and neurological conditions known to impact GI motility. Propensity score matching (1:1) was performed to balance both cohorts on key demographic and clinical variables, including age, gender, comorbidity index, BMI range, tobacco use, alcohol use, diabetes, and socioeconomic status. After matching, each cohort included 456,016 patients.
Results: Baseline demographic and clinical characteristics of the matched cohorts are summarized in Table 1. CVS was identified in 0.67% vs 0.10% [RR 6.5, CI (5.9, 7.19)], GP in 0.35% vs.0.15% [RR 2.399, CI (2.18, 2.62)] and IBD in 0.55% vs 0.93% [RR,0.538 CI (0.51, 0.57)] in cannabis users versus non-users respectively (all p < 0.001).
Discussion: This study demonstrates a significantly increased risk of CVS and GP among cannabis users compared to non-users in contrast to IBD which had a lower incidence. The directionality of these associations and whether cannabis causes or worsens vomiting or is used by CVS and GP patients due to a lack of targeted therapies is unclear. Limitations include the use of a database and retrospective coding. However, this is the largest study on this topic to our knowledge with ~ a million patients and further prospective research to better understand the effects of cannabis use on CVS and GP are warranted.
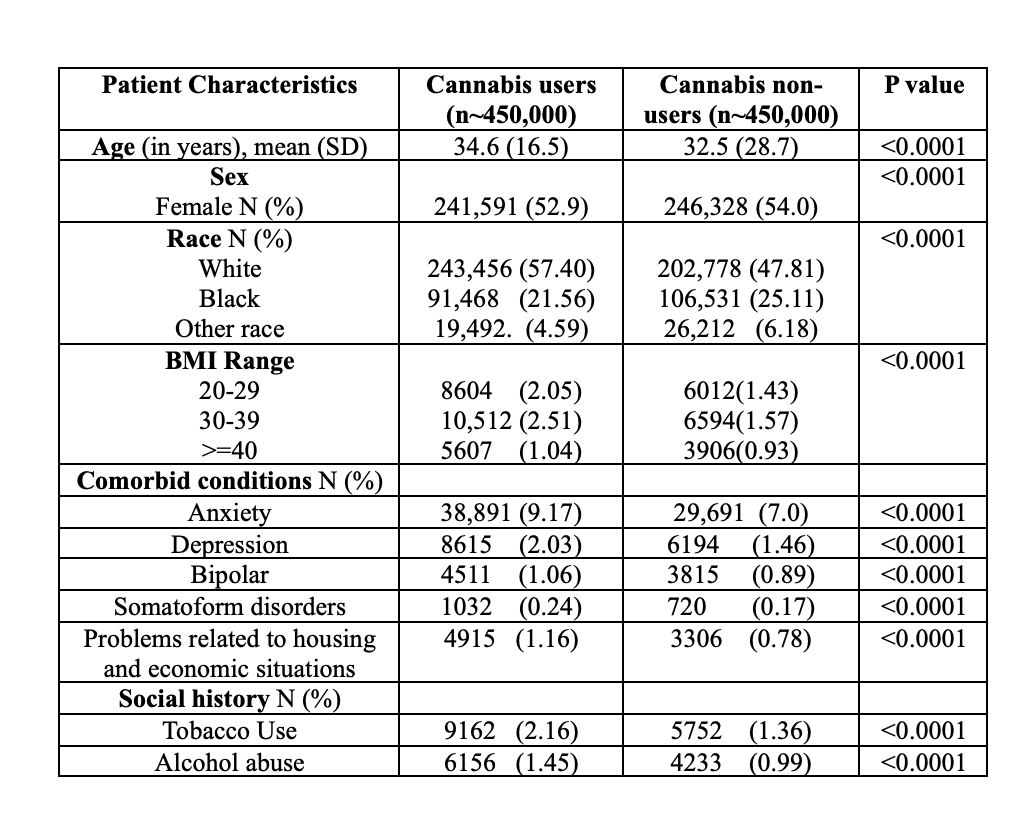
Figure: Table 1: Demographics and clinical characteristics of patients in matched cohorts
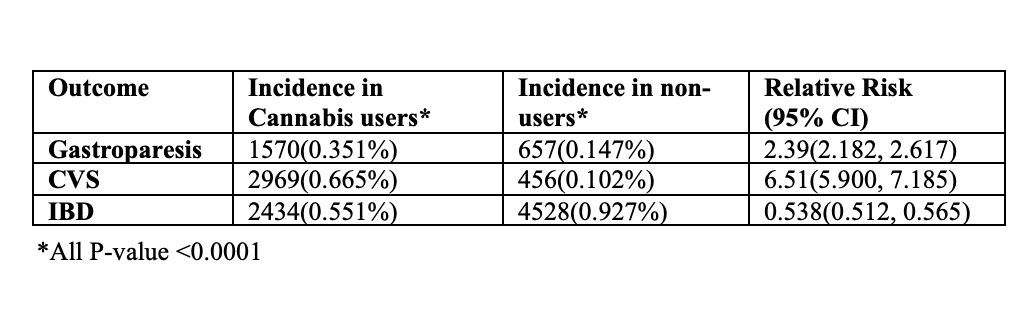
Figure: Table 2: Incidence and Relative Risk of Gp, CVS, and IBD Among Cannabis Users vs. Non-Users
Disclosures:
Saranya Arumugam indicated no relevant financial relationships.
Omayma Alshaarawy indicated no relevant financial relationships.
Khaled Al Smadi indicated no relevant financial relationships.
Thangam Venkatesan: Azurity – Consultant. Takeda Pharmaceuticals – Consultant, Grant/Research Support.
Saranya Arumugam, MD1, Omayma Alshaarawy, PhD2, Khaled Al Smadi, MD3, Thangam Venkatesan, MD4. P0819 - POSTER WITHDRAWN, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
