Sunday Poster Session
Category: General Endoscopy
P0855 - Diagnostic Performance of Artificial Intelligence Models in Detecting Helicobacter pylori Infection Through Upper Gastrointestinal Endoscopy: A Systematic Review and Meta-analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Has Audio

Ahmad Al Homaid, MD
Nazareth Hospital
Philadelphia, PA
Presenting Author(s)
Ahmad Alhomaid, MD1, Kaur Shreyjit, MBBS2, Pranav Patel, MD3, Mipasha Patel, MD4, Priyanka Mohnani, MD5, Rupak Desai, MBBS6, Bradley D. Confer, DO3, Harshit S. Khara, MD7
1Nazareth Hospital, Philadelphia, PA; 2Health Education Services/Flowers Hospital, Dothan, AL; 3Geisinger Health System, Danville, PA; 4Abington Jefferson Hospital, Willow Grove, PA; 5Parkview health, Schaumburg, IL; 6Independent Outcomes Researcher, Atlanta, GA; 7Geisinger Health System, Danville, NJ
Introduction: Helicobacter pylori (H. pylori) infection is a major cause of peptic ulcer disease, chronic gastritis and gastric cancer. Upper gastrointestinal endoscopy is an important diagnostic modality for diagnosing H. pylori infection. Its use can be enhanced using various Artificial Intelligence (AI) models. We aim to evaluate the diagnostic performance of AI models in detecting H. pylori infection through upper gastrointestinal endoscopy.
Methods: A comprehensive literature review was done over the PubMed, SCOPUS, and Google Scholar databases till November 2024. Studies employing AI-based approaches for H. pylori detection were included, excluding training datasets to reduce bias and focusing only on validation and testing datasets. Data from these studies was pooled to calculate Area Under the Receiver Operating Characteristic (AUROC), accuracy, sensitivity, and specificity using random-effects models. Subgroup and sensitivity analyses were also performed.
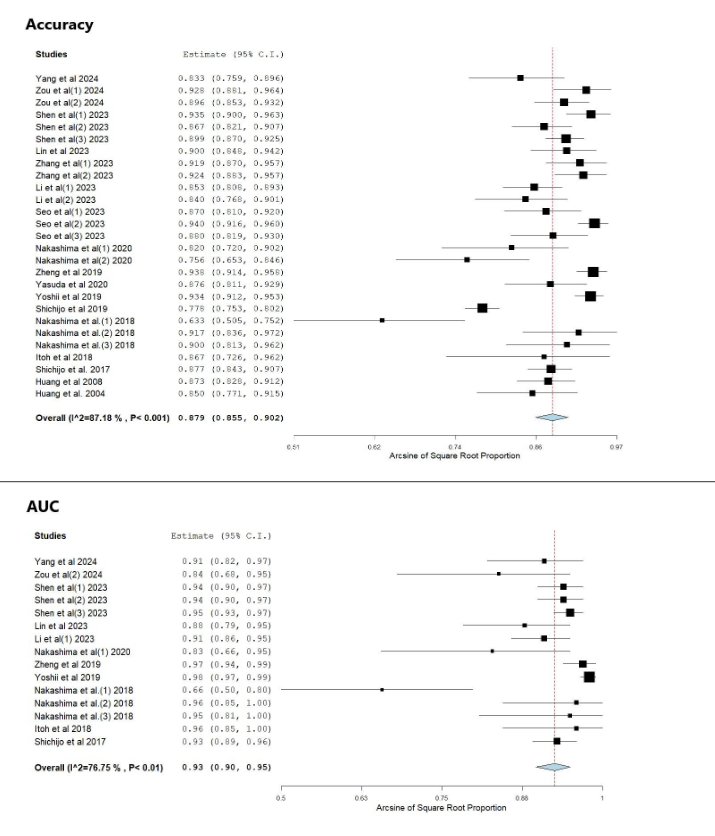
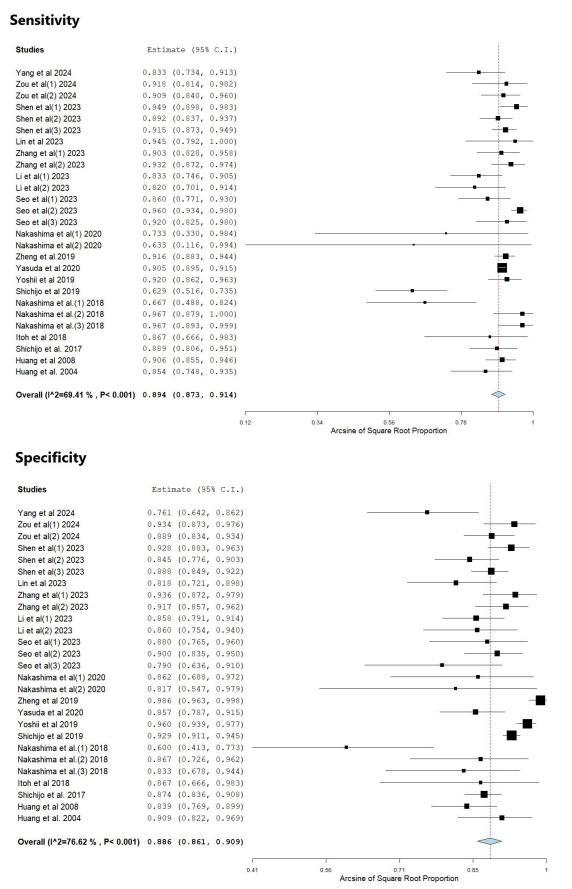
Results: Out of 71 initial studies, 17 studies were included in the final analysis: 5 randomized controlled trials (RCTs) and 12 observational studies. These studies evaluated AI models across 27 independent datasets. The pooled parameters calculated were: AUROC 0.93 (95% CI: 0.90–0.95), sensitivity 0.894 (95% CI: 0.873, 0.914), and specificity 0.886 (95% CI: 0.861, 0.909) and accuracy 0.879 (95% CI: 0.855, 0.902). Moderate heterogeneity was also observed (I2 = 69–77%) due to the variability amongst the studies. Despite variability, AI systems were consistent in differentiating between positive and negative H. pylori cases.
Discussion: This meta-analysis establishes that AI-based systems have excellent diagnostic performance in detecting H. pylori infection with high sensitivity, specificity and overall accuracy. Hence, there is a significant potential for their use into routine clinical practice. However, more research is required to validate these findings across diverse clinical settings.
Disclosures:
Ahmad Alhomaid, MD1, Kaur Shreyjit, MBBS2, Pranav Patel, MD3, Mipasha Patel, MD4, Priyanka Mohnani, MD5, Rupak Desai, MBBS6, Bradley D. Confer, DO3, Harshit S. Khara, MD7. P0855 - Diagnostic Performance of Artificial Intelligence Models in Detecting Helicobacter Pylori Infection Through Upper Gastrointestinal Endoscopy: A Systematic Review and Meta-analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Nazareth Hospital, Philadelphia, PA; 2Health Education Services/Flowers Hospital, Dothan, AL; 3Geisinger Health System, Danville, PA; 4Abington Jefferson Hospital, Willow Grove, PA; 5Parkview health, Schaumburg, IL; 6Independent Outcomes Researcher, Atlanta, GA; 7Geisinger Health System, Danville, NJ
Introduction: Helicobacter pylori (H. pylori) infection is a major cause of peptic ulcer disease, chronic gastritis and gastric cancer. Upper gastrointestinal endoscopy is an important diagnostic modality for diagnosing H. pylori infection. Its use can be enhanced using various Artificial Intelligence (AI) models. We aim to evaluate the diagnostic performance of AI models in detecting H. pylori infection through upper gastrointestinal endoscopy.
Methods: A comprehensive literature review was done over the PubMed, SCOPUS, and Google Scholar databases till November 2024. Studies employing AI-based approaches for H. pylori detection were included, excluding training datasets to reduce bias and focusing only on validation and testing datasets. Data from these studies was pooled to calculate Area Under the Receiver Operating Characteristic (AUROC), accuracy, sensitivity, and specificity using random-effects models. Subgroup and sensitivity analyses were also performed.
Results: Out of 71 initial studies, 17 studies were included in the final analysis: 5 randomized controlled trials (RCTs) and 12 observational studies. These studies evaluated AI models across 27 independent datasets. The pooled parameters calculated were: AUROC 0.93 (95% CI: 0.90–0.95), sensitivity 0.894 (95% CI: 0.873, 0.914), and specificity 0.886 (95% CI: 0.861, 0.909) and accuracy 0.879 (95% CI: 0.855, 0.902). Moderate heterogeneity was also observed (I2 = 69–77%) due to the variability amongst the studies. Despite variability, AI systems were consistent in differentiating between positive and negative H. pylori cases.
Discussion: This meta-analysis establishes that AI-based systems have excellent diagnostic performance in detecting H. pylori infection with high sensitivity, specificity and overall accuracy. Hence, there is a significant potential for their use into routine clinical practice. However, more research is required to validate these findings across diverse clinical settings.
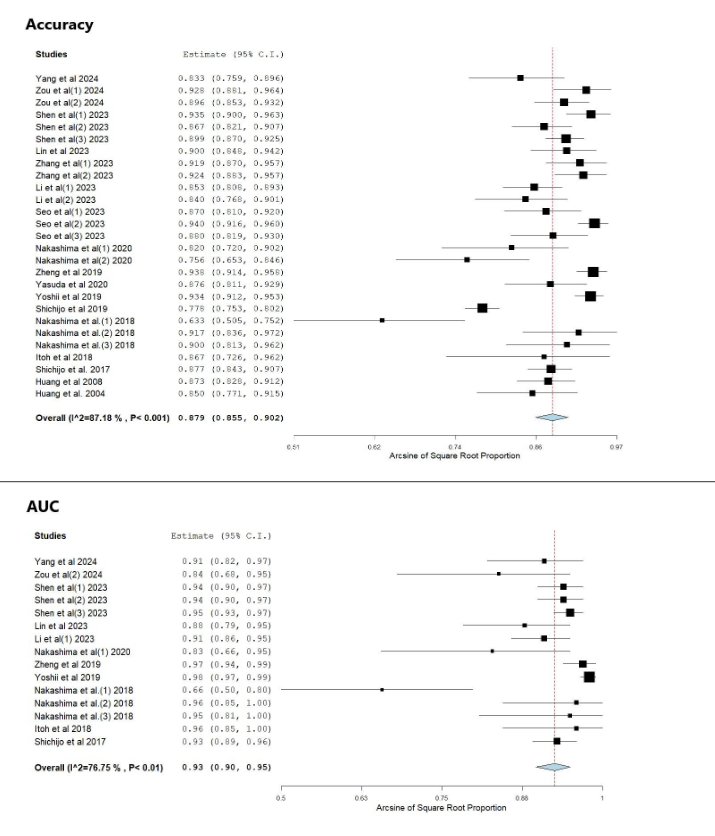
Figure: Forest plots showing diagnostic performance metrics. (Top) Accuracy from 24 studies with pooled estimate of 0.879 (95% CI: 0.855-0.902). (Bottom) AUC from 15 studies with pooled estimate of 0.93 (95% CI: 0.90-0.95). Both analyses show high heterogeneity with I²>75%.
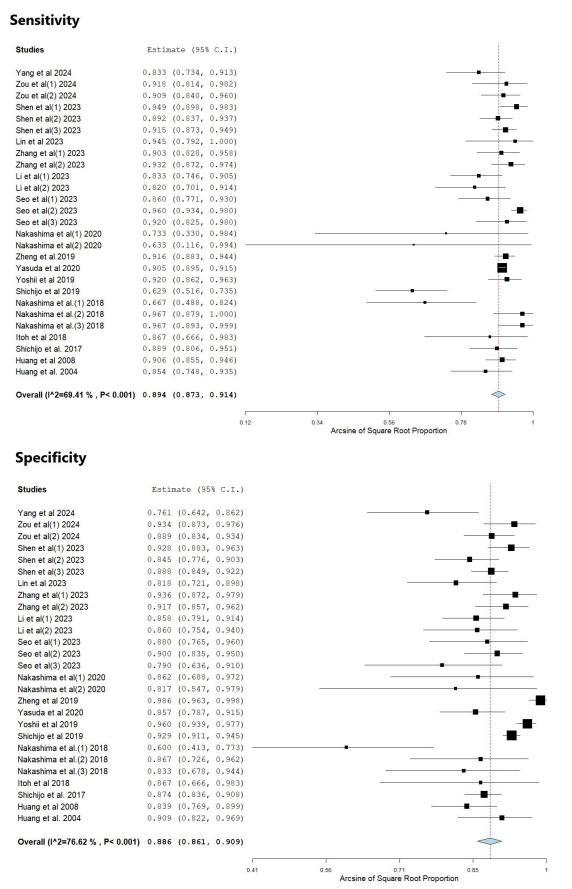
Figure: Forest plots of diagnostic test performance. (Top) Sensitivity from 25 studies with pooled estimate of 0.894 (95% CI: 0.873-0.914, I²=89.1%). (Bottom) Specificity from 25 studies with pooled estimate of 0.886 (95% CI: 0.861-0.909, I²=76.5%). Both metrics show high heterogeneity across studies.
Disclosures:
Ahmad Alhomaid indicated no relevant financial relationships.
Kaur Shreyjit indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Mipasha Patel indicated no relevant financial relationships.
Priyanka Mohnani indicated no relevant financial relationships.
Rupak Desai indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
Ahmad Alhomaid, MD1, Kaur Shreyjit, MBBS2, Pranav Patel, MD3, Mipasha Patel, MD4, Priyanka Mohnani, MD5, Rupak Desai, MBBS6, Bradley D. Confer, DO3, Harshit S. Khara, MD7. P0855 - Diagnostic Performance of Artificial Intelligence Models in Detecting Helicobacter Pylori Infection Through Upper Gastrointestinal Endoscopy: A Systematic Review and Meta-analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
