Sunday Poster Session
Category: Infections and Microbiome
P1304 - The Price of Infection: Increased Morbidity, Mortality, and Costs Associated With Clostridiodies difficile Infection Among GI-Related Cancer Patients in the US
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Has Audio

Timothy Davie, MD
University of Minnesota Medical Center
Minneapolis, MN
Presenting Author(s)
Timothy Davie, MD1, Giovanni Roldan Carrillo, MD2, Spencer Goble, MD3, Jesse Fletcher, MD2, Daphne Moutsoglou, MD, PhD4
1University of Minnesota Medical Center, Minneapolis, MN; 2University of Minnesota Medical School, Minneapolis, MN; 3University of Minnesota, Minneapolis, MN; 4University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Patients with cancer have a higher risk of developing Clostridiodies difficile infection (CDI). Gastrointestinal cancers comprise about 25% of all cancers worldwide. However, recent, population-level studies assessing the burden of CDI outcomes in patients with GI cancer in the U.S remain limited. We evaluated the morbidity and mortality among GI cancer patients with CDI using a nationwide inpatient database.
Methods: Using data from the National Inpatient Sample from 2016-2022, we performed a retrospective cross-sectional analysis that focused on admissions for patients with a GI-related cancer (esophageal, colorectal, gastric, liver, pancreatic, and other related cancer types). Patient demographics, in-hospital death, clinical utilization outcomes, and costs were compared between GI cancer patients with and without CDI. CDI odds and outcomes measures were compared between GI cancer subtypes. We adjusted for patient and hospital-level factors using multivariable logistic regression models.
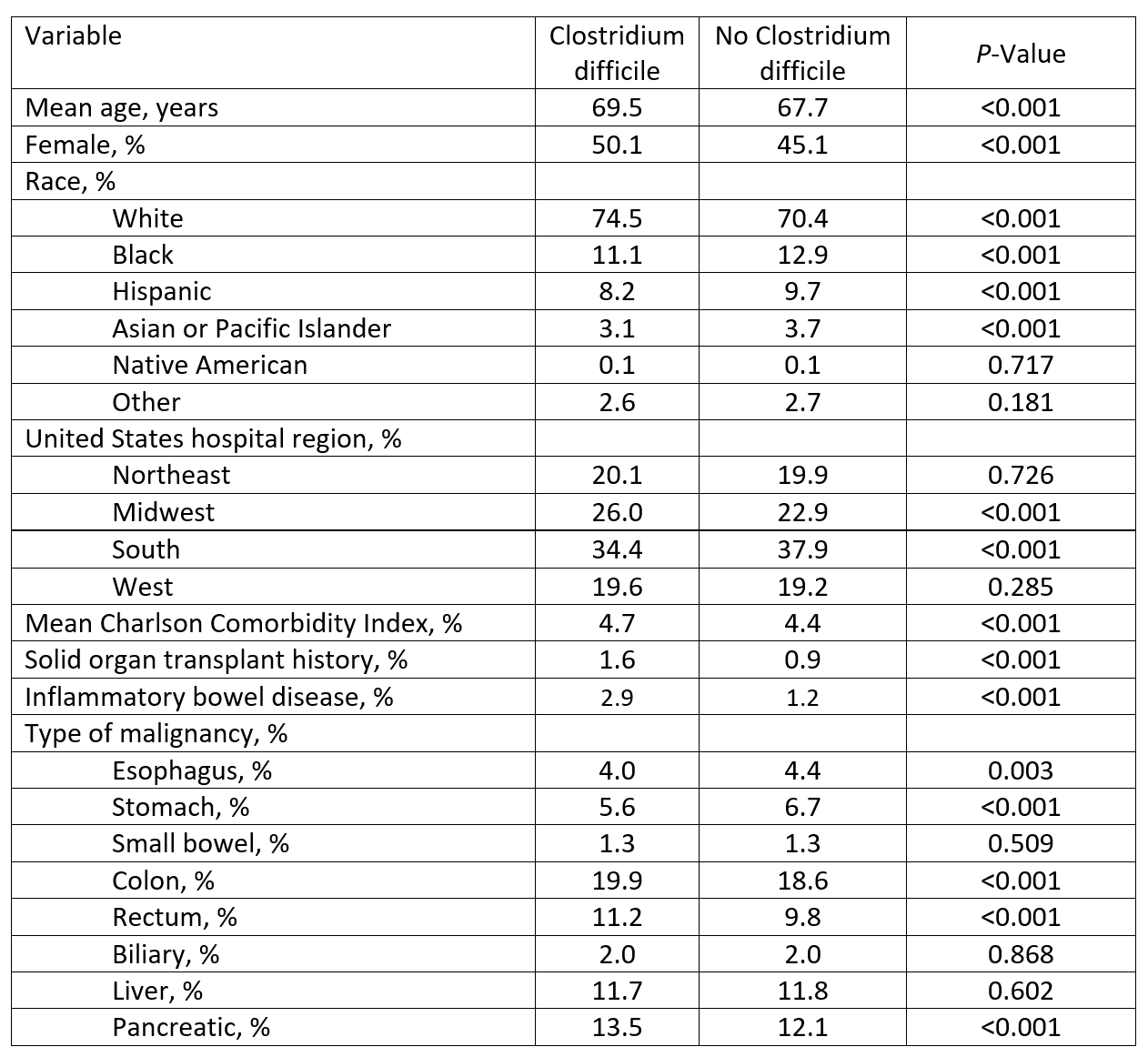
Results: Among 6,409,668 GI cancer-related admissions in the U.S., 92,765 patients were diagnosed with CDI. Patients diagnosed with CDI tended to be female (50.5% vs 45.1%, p< 0.001), of older age (mean 69.5 vs 68.7 years, p< 0.001), with a high comorbidity burden (mean Charlson Comorbidity Index of 4.7 vs 4.4, p< 0.001) (Table 1). GI cancer patients with CDI had increased in-hospital mortality (aOR = 1.36, 95% CI: 1.28-1.45, p< 0.001) and increased utilization of renal replacement therapy (aOR = 2.14, 95% CI: 1.97-2.32, p< 0.001), mechanical ventilation (aOR = 1.83, 95% CI: 1.72-1.95, p< 0.001), and vasopressors (aOR = 1.85, 95% CI: 1.66-2.06, p< 0.001). Hospital stays were longer for GI cancer patients with CDI (mean 9.8 vs 5.9 days, p< 0.001) and cost was increased ($18,102 vs $7,100, p< 0.001). Among GI cancer subtypes, rectal cancer had the highest CDI incidence (1.7%), followed by pancreatic cancer (1.6%). Esophageal cancer patients with CDI had the highest mortality (12.3%), followed by biliary cancer patients (10.2%). Geographically, mortality was highest among GI cancer patients with CDI in the U.S. West (7.8%) and lowest in the Midwest (5.7%).
Discussion: Using national data, we found that patients with GI cancer diagnosed with CDI have increased morbidity and mortality, longer hospital stays, and higher hospitalization costs. Implementation of infection prevention strategies and greater awareness of the risks associated with CDI infection may improve clinical outcomes for GI cancer patients.
Disclosures:
Timothy Davie, MD1, Giovanni Roldan Carrillo, MD2, Spencer Goble, MD3, Jesse Fletcher, MD2, Daphne Moutsoglou, MD, PhD4. P1304 - The Price of Infection: Increased Morbidity, Mortality, and Costs Associated With <i>Clostridiodies difficile</i> Infection Among GI-Related Cancer Patients in the US, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Minnesota Medical Center, Minneapolis, MN; 2University of Minnesota Medical School, Minneapolis, MN; 3University of Minnesota, Minneapolis, MN; 4University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Patients with cancer have a higher risk of developing Clostridiodies difficile infection (CDI). Gastrointestinal cancers comprise about 25% of all cancers worldwide. However, recent, population-level studies assessing the burden of CDI outcomes in patients with GI cancer in the U.S remain limited. We evaluated the morbidity and mortality among GI cancer patients with CDI using a nationwide inpatient database.
Methods: Using data from the National Inpatient Sample from 2016-2022, we performed a retrospective cross-sectional analysis that focused on admissions for patients with a GI-related cancer (esophageal, colorectal, gastric, liver, pancreatic, and other related cancer types). Patient demographics, in-hospital death, clinical utilization outcomes, and costs were compared between GI cancer patients with and without CDI. CDI odds and outcomes measures were compared between GI cancer subtypes. We adjusted for patient and hospital-level factors using multivariable logistic regression models.
Results: Among 6,409,668 GI cancer-related admissions in the U.S., 92,765 patients were diagnosed with CDI. Patients diagnosed with CDI tended to be female (50.5% vs 45.1%, p< 0.001), of older age (mean 69.5 vs 68.7 years, p< 0.001), with a high comorbidity burden (mean Charlson Comorbidity Index of 4.7 vs 4.4, p< 0.001) (Table 1). GI cancer patients with CDI had increased in-hospital mortality (aOR = 1.36, 95% CI: 1.28-1.45, p< 0.001) and increased utilization of renal replacement therapy (aOR = 2.14, 95% CI: 1.97-2.32, p< 0.001), mechanical ventilation (aOR = 1.83, 95% CI: 1.72-1.95, p< 0.001), and vasopressors (aOR = 1.85, 95% CI: 1.66-2.06, p< 0.001). Hospital stays were longer for GI cancer patients with CDI (mean 9.8 vs 5.9 days, p< 0.001) and cost was increased ($18,102 vs $7,100, p< 0.001). Among GI cancer subtypes, rectal cancer had the highest CDI incidence (1.7%), followed by pancreatic cancer (1.6%). Esophageal cancer patients with CDI had the highest mortality (12.3%), followed by biliary cancer patients (10.2%). Geographically, mortality was highest among GI cancer patients with CDI in the U.S. West (7.8%) and lowest in the Midwest (5.7%).
Discussion: Using national data, we found that patients with GI cancer diagnosed with CDI have increased morbidity and mortality, longer hospital stays, and higher hospitalization costs. Implementation of infection prevention strategies and greater awareness of the risks associated with CDI infection may improve clinical outcomes for GI cancer patients.
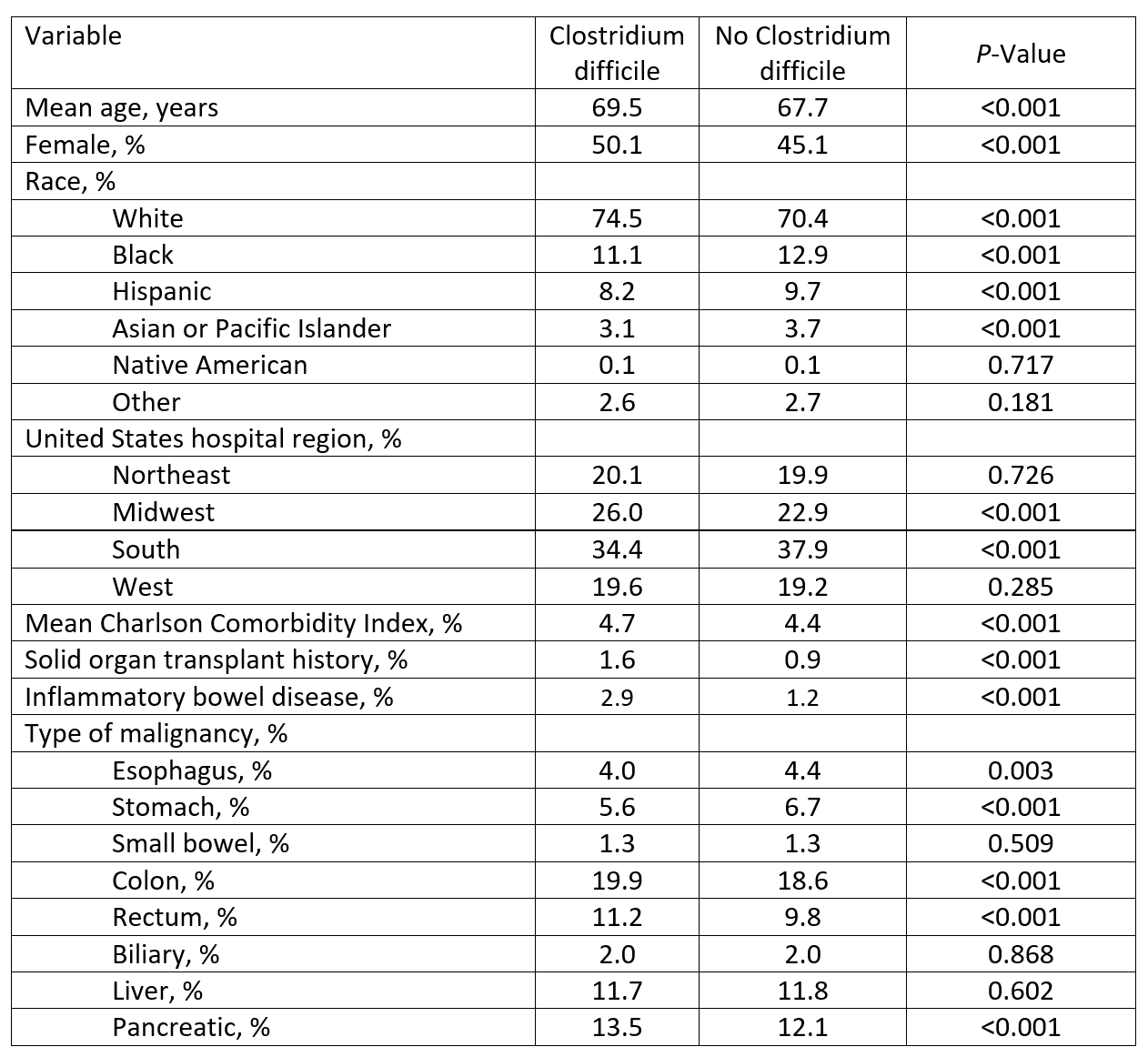
Figure: Table 1. Characteristics of patients with GI malignancy-related hospitalizations stratified by the presence of Clostridium difficile infection
Disclosures:
Timothy Davie indicated no relevant financial relationships.
Giovanni Roldan Carrillo indicated no relevant financial relationships.
Spencer Goble indicated no relevant financial relationships.
Jesse Fletcher indicated no relevant financial relationships.
Daphne Moutsoglou indicated no relevant financial relationships.
Timothy Davie, MD1, Giovanni Roldan Carrillo, MD2, Spencer Goble, MD3, Jesse Fletcher, MD2, Daphne Moutsoglou, MD, PhD4. P1304 - The Price of Infection: Increased Morbidity, Mortality, and Costs Associated With <i>Clostridiodies difficile</i> Infection Among GI-Related Cancer Patients in the US, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
