Sunday Poster Session
Category: Infections and Microbiome
P1305 - KRAS Mutations Set the Stage for Enterotoxigenic Bacteroides fragilis-Induced Sepsis in Pancreatic and Colorectal Cancer
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Has Audio

Allen Luo, MD
Keck School of Medicine of the University of Southern California, CA
Presenting Author(s)
Allen Luo, MD1, Allen Seylani, MD2, Yohannes Haile, MD2, Assal Sadighian, BS2, Sadaf Sadighian, BS2
1Keck School of Medicine of the University of Southern California, Moorpark, CA; 2University of California Riverside School of Medicine, Riverside, CA
Introduction: Pancreatic cancer ranks as the sixth leading cause of cancer death worldwide; colorectal cancer is the second deadliest globally. KRAS mutations occur in ~80% of all pancreatic cancers and in 45% of colorectal cancers. These mutations, especially the KRAS G12D variant, cause a heightened inflammatory state leading to susceptibility to Enterotoxigenic Bacteroides fragilis (ETBF), a commensal bacterium that produces a toxin that disrupts epithelial tight junctions and drives inflammation. In combination, these factors may increase the risk of septic shock.
Methods: We conducted a retrospective cohort study utilizing de-identified patient data from the TriNetX platform, a comprehensive electronic health records system consisting of 143 healthcare systems from 18 countries and over 163 million patients' records. In this study, we compare the risk of sepsis for patients with positive blood cultures for ETBF and KRAS-associated pancreatic cancer (Cohort A) versus KRAS-associated colorectal cancer (Cohort B). Additionally, we analyzed post-sepsis outcomes, deep vein thrombosis (DVT) and pulmonary embolism (PE).
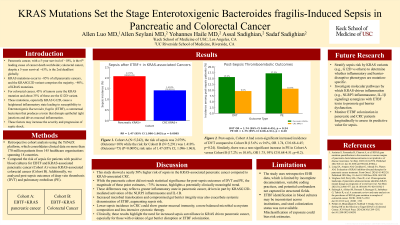
Results: For Cohort A (N=5,242), the risk of sepsis was 2.1% (N=109) while the risk for Cohort B (N=5,291) was 1.4% (N=75) (P=0.01), corresponding to a risk ratio of 1.5 (95% CI, 1.10-1.96). Post-sepsis, Cohort A had a non-significant increased incidence of DVT compared to Cohort B (15.6% vs 9.6%, OR 1.7, CI 0.7-4.4; p=0.2). Similarly, there was a non-significant increase in PE in Cohort A (17.2% vs 10.6%, OR 1.8, 95% CI 0.7-4.5; p=0.2).
Discussion: This study showed a nearly 50% higher risk of sepsis in the KRAS-associated pancreatic cancer compared to KRAS-associated CRC. While the pancreatic cohort did not reach significance for DVT and PE, the magnitude of these measures, ~75% increase in both, highlights a potentially meaningful trend. These differences may reflect a greater inflammatory state in pancreatic cancer, driven in part by KRASG12D-mediated activation of the NLRP3 inflammasome and IL-1B. Increased microbial translocation and compromised gut barrier integrity may also exacerbate systemic dissemination of ETBF. Conversely, lower sepsis incidence in CRC could show greater mucosal immunity, a more balanced microbial ecosystem composition and less intensive chemotherapy. Clinically, these results highlight the need for increased sepsis surveillance in KRAS pancreatic cancer, especially for those with evidence of gut barrier disruption or ETBF colonization.
Disclosures:
Allen Luo, MD1, Allen Seylani, MD2, Yohannes Haile, MD2, Assal Sadighian, BS2, Sadaf Sadighian, BS2. P1305 - KRAS Mutations Set the Stage for Enterotoxigenic <i>Bacteroides fragilis</i>-Induced Sepsis in Pancreatic and Colorectal Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Keck School of Medicine of the University of Southern California, Moorpark, CA; 2University of California Riverside School of Medicine, Riverside, CA
Introduction: Pancreatic cancer ranks as the sixth leading cause of cancer death worldwide; colorectal cancer is the second deadliest globally. KRAS mutations occur in ~80% of all pancreatic cancers and in 45% of colorectal cancers. These mutations, especially the KRAS G12D variant, cause a heightened inflammatory state leading to susceptibility to Enterotoxigenic Bacteroides fragilis (ETBF), a commensal bacterium that produces a toxin that disrupts epithelial tight junctions and drives inflammation. In combination, these factors may increase the risk of septic shock.
Methods: We conducted a retrospective cohort study utilizing de-identified patient data from the TriNetX platform, a comprehensive electronic health records system consisting of 143 healthcare systems from 18 countries and over 163 million patients' records. In this study, we compare the risk of sepsis for patients with positive blood cultures for ETBF and KRAS-associated pancreatic cancer (Cohort A) versus KRAS-associated colorectal cancer (Cohort B). Additionally, we analyzed post-sepsis outcomes, deep vein thrombosis (DVT) and pulmonary embolism (PE).
Results: For Cohort A (N=5,242), the risk of sepsis was 2.1% (N=109) while the risk for Cohort B (N=5,291) was 1.4% (N=75) (P=0.01), corresponding to a risk ratio of 1.5 (95% CI, 1.10-1.96). Post-sepsis, Cohort A had a non-significant increased incidence of DVT compared to Cohort B (15.6% vs 9.6%, OR 1.7, CI 0.7-4.4; p=0.2). Similarly, there was a non-significant increase in PE in Cohort A (17.2% vs 10.6%, OR 1.8, 95% CI 0.7-4.5; p=0.2).
Discussion: This study showed a nearly 50% higher risk of sepsis in the KRAS-associated pancreatic cancer compared to KRAS-associated CRC. While the pancreatic cohort did not reach significance for DVT and PE, the magnitude of these measures, ~75% increase in both, highlights a potentially meaningful trend. These differences may reflect a greater inflammatory state in pancreatic cancer, driven in part by KRASG12D-mediated activation of the NLRP3 inflammasome and IL-1B. Increased microbial translocation and compromised gut barrier integrity may also exacerbate systemic dissemination of ETBF. Conversely, lower sepsis incidence in CRC could show greater mucosal immunity, a more balanced microbial ecosystem composition and less intensive chemotherapy. Clinically, these results highlight the need for increased sepsis surveillance in KRAS pancreatic cancer, especially for those with evidence of gut barrier disruption or ETBF colonization.
Disclosures:
Allen Luo indicated no relevant financial relationships.
Allen Seylani indicated no relevant financial relationships.
Yohannes Haile indicated no relevant financial relationships.
Assal Sadighian indicated no relevant financial relationships.
Sadaf Sadighian indicated no relevant financial relationships.
Allen Luo, MD1, Allen Seylani, MD2, Yohannes Haile, MD2, Assal Sadighian, BS2, Sadaf Sadighian, BS2. P1305 - KRAS Mutations Set the Stage for Enterotoxigenic <i>Bacteroides fragilis</i>-Induced Sepsis in Pancreatic and Colorectal Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
