Sunday Poster Session
Category: Infections and Microbiome
P1329 - Fulminant C. difficile Colitis Mimicking Typhlitis in a Patient Undergoing BiTE Therapy: Diagnostic and Therapeutic Challenges in a Neutropenic Host
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Has Audio

Alicia Gorin, MD
Beth Israel Deaconess Medical Center, Harvard Medical School
Boston, Massachusetts
Presenting Author(s)
Aman Mohapatra, MD1, Alicia Gorin, MD2
1Beth Israel Deaconess Medical Center, Harvard Medical School, Folsom, CA; 2Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
Introduction: Typhlitis is a well-known complication in immunocompromised patients presenting with right-sided abdominal pain and neutropenia. However, fulminant Clostridioides difficile infection (CDI) can initially present similarly, particularly in patients without diarrhea. We present a diagnostically challenging case of fulminant CDI mimicking typhlitis in a neutropenic patient undergoing bispecific T-cell engager (BiTE) therapy.
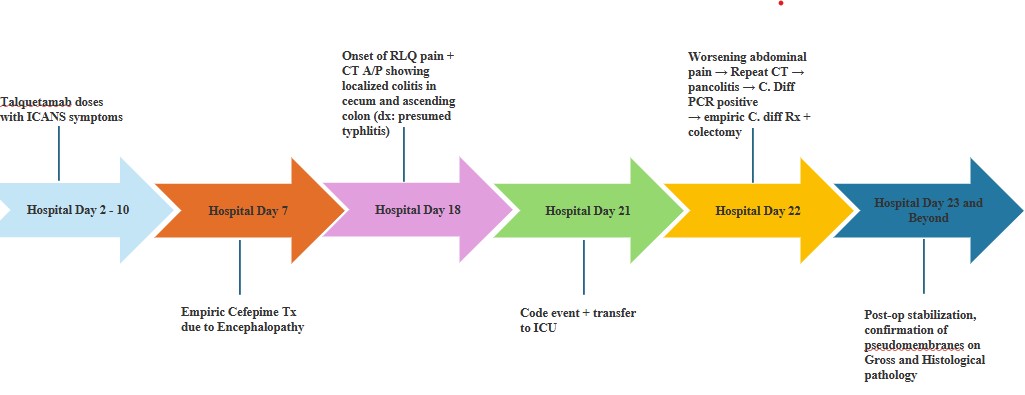
Case Description/Methods: A 65-year-old male with multiple myeloma was admitted for Talquetamab ramp-up in preparation for CAR-T. After each dose, he developed progressive altered mental status consistent with Immune Effector Cell-associated Neurotoxicity Syndrome (ICANS), treated with dexamethasone. He was started on empiric cefepime on Hospital Day 7 due to neutropenia (Figure 1) and concern for infectious encephalopathy—an established risk factor for CDI. On Day 18, he developed right lower quadrant pain without diarrhea. He was hemodynamically stable but neutropenic. CT imaging showed cecal and ascending colitis, concerning for typhlitis, prompting antibiotic broadening for anaerobic coverage.
On Day 21, he was transferred to the ICU for worsening ICANS. He remained tenuous with increasing abdominal pain and rebound tenderness. Repeat CT showed pancolitis, raising concern for fulminant colitis. Despite only one loose stool, CDI PCR was sent (outside institutional criteria), and he was empirically started on oral/rectal vancomycin and IV metronidazole. GI, ID, and surgical services were consulted. Due to rising lactate, worsening vitals, and imaging suggestive of toxic megacolon, he underwent emergent total colectomy. Postoperatively, he stabilized. Pathology confirmed pseudomembranous colitis without features of typhlitis.
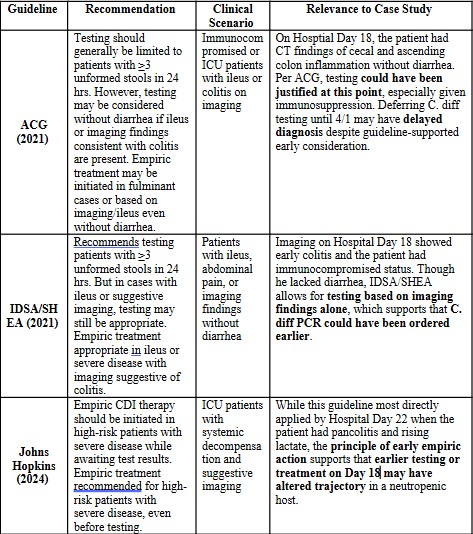
Discussion: This case highlights the need for clinical judgment in complex immunocompromised patients. Though right-sided colitis in neutropenic hosts suggests typhlitis, early CDI must be considered, particularly with recent antibiotic exposure (Table 1). Strict reliance on ≥3 loose stools for CDI testing may delay diagnosis in critically ill patients. Here, imaging and systemic decline guided empiric therapy and testing, which proved lifesaving. Steroid use for ICANS complicated decisions, as corticosteroids are generally contraindicated in infectious colitis. Multidisciplinary ICU management enabled timely diagnosis, surgery, and recovery despite fulminant disease in a pancytopenic patient.
Disclosures:
Aman Mohapatra, MD1, Alicia Gorin, MD2. P1329 - Fulminant C. difficile Colitis Mimicking Typhlitis in a Patient Undergoing BiTE Therapy: Diagnostic and Therapeutic Challenges in a Neutropenic Host, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Beth Israel Deaconess Medical Center, Harvard Medical School, Folsom, CA; 2Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
Introduction: Typhlitis is a well-known complication in immunocompromised patients presenting with right-sided abdominal pain and neutropenia. However, fulminant Clostridioides difficile infection (CDI) can initially present similarly, particularly in patients without diarrhea. We present a diagnostically challenging case of fulminant CDI mimicking typhlitis in a neutropenic patient undergoing bispecific T-cell engager (BiTE) therapy.
Case Description/Methods: A 65-year-old male with multiple myeloma was admitted for Talquetamab ramp-up in preparation for CAR-T. After each dose, he developed progressive altered mental status consistent with Immune Effector Cell-associated Neurotoxicity Syndrome (ICANS), treated with dexamethasone. He was started on empiric cefepime on Hospital Day 7 due to neutropenia (Figure 1) and concern for infectious encephalopathy—an established risk factor for CDI. On Day 18, he developed right lower quadrant pain without diarrhea. He was hemodynamically stable but neutropenic. CT imaging showed cecal and ascending colitis, concerning for typhlitis, prompting antibiotic broadening for anaerobic coverage.
On Day 21, he was transferred to the ICU for worsening ICANS. He remained tenuous with increasing abdominal pain and rebound tenderness. Repeat CT showed pancolitis, raising concern for fulminant colitis. Despite only one loose stool, CDI PCR was sent (outside institutional criteria), and he was empirically started on oral/rectal vancomycin and IV metronidazole. GI, ID, and surgical services were consulted. Due to rising lactate, worsening vitals, and imaging suggestive of toxic megacolon, he underwent emergent total colectomy. Postoperatively, he stabilized. Pathology confirmed pseudomembranous colitis without features of typhlitis.
Discussion: This case highlights the need for clinical judgment in complex immunocompromised patients. Though right-sided colitis in neutropenic hosts suggests typhlitis, early CDI must be considered, particularly with recent antibiotic exposure (Table 1). Strict reliance on ≥3 loose stools for CDI testing may delay diagnosis in critically ill patients. Here, imaging and systemic decline guided empiric therapy and testing, which proved lifesaving. Steroid use for ICANS complicated decisions, as corticosteroids are generally contraindicated in infectious colitis. Multidisciplinary ICU management enabled timely diagnosis, surgery, and recovery despite fulminant disease in a pancytopenic patient.
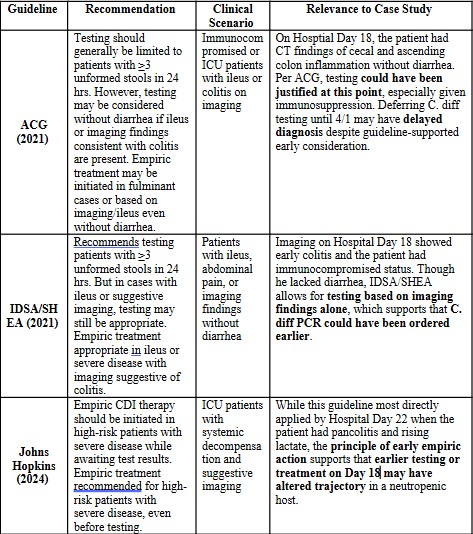
Figure: Figure 1. Timeline of Key Clinical Events : Admission for Talquetamab ramp-up for CAR-T therapy in a Multiple Myeloma Patient . A visual overview of the patient's clinical progression from Talquetamab administration and antibiotic initiation to onset of abdominal symptoms, ICU transfer, surgical intervention, and final diagnosis. This timeline highlights diagnostic inflection points, therapeutic decisions, and the evolving presentation of fulminant C. difficile colitis.
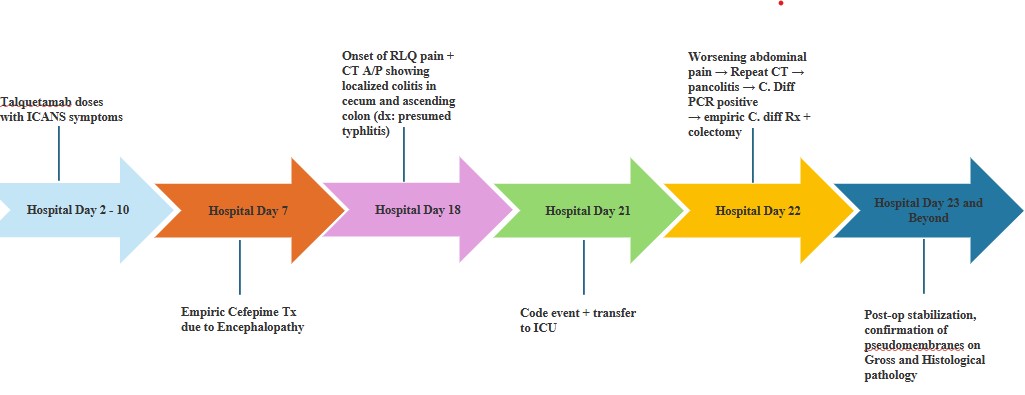
Figure: Table 1. Guideline Recommendations on CDI Testing/Treatment Without Diarrhea - Illustrates key guideline-based recommendations from ACG, IDSA/SHEA, and Johns Hopkins for initiating C. difficile testing or empiric treatment in high-risk patients without diarrhea. The case presented aligns with exceptions supported by these guidelines, where early imaging and immunocompromised status justified lower testing thresholds.
Disclosures:
Aman Mohapatra indicated no relevant financial relationships.
Alicia Gorin indicated no relevant financial relationships.
Aman Mohapatra, MD1, Alicia Gorin, MD2. P1329 - Fulminant C. difficile Colitis Mimicking Typhlitis in a Patient Undergoing BiTE Therapy: Diagnostic and Therapeutic Challenges in a Neutropenic Host, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
