Sunday Poster Session
Category: Infections and Microbiome
P1331 - Rare Presentation of Small Bowel Necrosis in the Setting of Fulminant Clostridioides difficile Infection After GLP-1 Usage
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Has Audio

Abigail L. Carroll, DO
Oklahoma State University Center for Health Sciences
Tulsa, OK
Presenting Author(s)
Abigail L. Carroll, DO, Andrew Harris, DO
Oklahoma State University Center for Health Sciences, Tulsa, OK
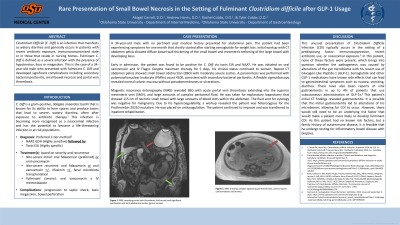
Introduction: Clostridium Difficile (C. Diff) is an infection that manifests as watery diarrhea and generally occurs in patients with recent antibiotic exposure, immunocompromised state or in those that reside in nursing homes. Fulminant C. Diff is defined as a severe infection with the presence of hypotension, ileus or megacolon. This is the case of a 34 year old male who presented with fulminant C. Diff and developed significant complications including secondary bacterial peritonitis, small bowel necrosis and portal vein thrombosis.
Case Description/Methods: A 34-year-old male with no pertinent past medical history presented to the emergency department (ER) for abdominal pain. The patient had been experiencing symptoms for one month that shortly started after using semaglutide. In the ER, workup with CT abdomen pelvis showed diffuse bowel wall thickening of the small bowel and mesenteric tethering of the large bowel with developing ileus.
Early in admission, the patient was found to be positive for C. diff. He was initiated on oral vancomycin and IV Flagyl. Despite maximum therapy, his clinical status continued to worsen. Repeat CT abdomen pelvis showed small bowel obstruction (SBO) with moderate-severe ascites. A paracentesis was performed with cell count 4100, consistent with spontaneous bacterial peritonitis. A flexible sigmoidoscopy then revealed normal colonic mucosa without pseudomembranes.
Magnetic resonance enterography (MRE) revealed SBO with acute portal vein thrombosis extending into the superior mesenteric vein (SMV), and large amounts of complex peritoneal fluid. He was taken for exploratory laparotomy that showed 115 cm of necrotic small bowel with large amounts of blood clots within the abdomen. The fluid sent for cytology was negative for malignancy. Due to his hypercoagulability, a workup revealed the patient was heterozygous for the Prothrombin 20210 mutation. On maximum therapy, the patient improved and was transferred to inpatient rehabilitation.
Discussion: This unusual presentation of C. diff brings into question whether the pathogenesis was caused by alterations of the gut microbiome with the patient's recent use of semaglutide. Semaglutide and other glucagon-like peptide (GLP-1) medications have known reports of viral gastroenteritis in up to 4% of patients that use subcutaneous administration. This gastroenteritis may have led to alterations of the patient's microbiome, allowing for the bacteria to grow and expand into fulminant infection, causing his extensive complications.
Disclosures:
Abigail L. Carroll, DO, Andrew Harris, DO. P1331 - Rare Presentation of Small Bowel Necrosis in the Setting of Fulminant <i>Clostridioides difficile</i> Infection After GLP-1 Usage, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Oklahoma State University Center for Health Sciences, Tulsa, OK
Introduction: Clostridium Difficile (C. Diff) is an infection that manifests as watery diarrhea and generally occurs in patients with recent antibiotic exposure, immunocompromised state or in those that reside in nursing homes. Fulminant C. Diff is defined as a severe infection with the presence of hypotension, ileus or megacolon. This is the case of a 34 year old male who presented with fulminant C. Diff and developed significant complications including secondary bacterial peritonitis, small bowel necrosis and portal vein thrombosis.
Case Description/Methods: A 34-year-old male with no pertinent past medical history presented to the emergency department (ER) for abdominal pain. The patient had been experiencing symptoms for one month that shortly started after using semaglutide. In the ER, workup with CT abdomen pelvis showed diffuse bowel wall thickening of the small bowel and mesenteric tethering of the large bowel with developing ileus.
Early in admission, the patient was found to be positive for C. diff. He was initiated on oral vancomycin and IV Flagyl. Despite maximum therapy, his clinical status continued to worsen. Repeat CT abdomen pelvis showed small bowel obstruction (SBO) with moderate-severe ascites. A paracentesis was performed with cell count 4100, consistent with spontaneous bacterial peritonitis. A flexible sigmoidoscopy then revealed normal colonic mucosa without pseudomembranes.
Magnetic resonance enterography (MRE) revealed SBO with acute portal vein thrombosis extending into the superior mesenteric vein (SMV), and large amounts of complex peritoneal fluid. He was taken for exploratory laparotomy that showed 115 cm of necrotic small bowel with large amounts of blood clots within the abdomen. The fluid sent for cytology was negative for malignancy. Due to his hypercoagulability, a workup revealed the patient was heterozygous for the Prothrombin 20210 mutation. On maximum therapy, the patient improved and was transferred to inpatient rehabilitation.
Discussion: This unusual presentation of C. diff brings into question whether the pathogenesis was caused by alterations of the gut microbiome with the patient's recent use of semaglutide. Semaglutide and other glucagon-like peptide (GLP-1) medications have known reports of viral gastroenteritis in up to 4% of patients that use subcutaneous administration. This gastroenteritis may have led to alterations of the patient's microbiome, allowing for the bacteria to grow and expand into fulminant infection, causing his extensive complications.
Disclosures:
Abigail Carroll indicated no relevant financial relationships.
Andrew Harris indicated no relevant financial relationships.
Abigail L. Carroll, DO, Andrew Harris, DO. P1331 - Rare Presentation of Small Bowel Necrosis in the Setting of Fulminant <i>Clostridioides difficile</i> Infection After GLP-1 Usage, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
