Tuesday Poster Session
Category: Colon
P4582 - Predictors of Ostomy and Outcomes in Colonic Stenting for Obstructing Colon Cancer

- RV
Renuka Verma, MD
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas
Las Vegas, NV
Presenting Author(s)
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 3Independent researcher, Las Vegas, NV; 4University of Pittsburgh, Newtown, PA
Introduction:
In colonic stenting, a self-expandable metallic stent (SEMS) is introduced in
the colon to alleviate the obstruction. However, in some cases, the need for ostomy may arise, impacting
their survival. Patients with colon cancer are at risk of intestinal obstruction, which may necessitate such
interventions. This study aimed to evaluate the incidence of ostomy among colonic stenting procedures in
colon cancer patients, factors that contributed to such procedures, and their all-cause-in-hospital death rate.
Methods:
Adults with colon cancer and suffering from intestinal obstruction who were hospitalized for
colonic stenting were studied through de-identified records compiled as the National Inpatient Sample. A
multivariable logistic regression model was created to analyze various factors that could have influenced the
need for ostomy creation. The mortality rate among those undergoing ostomy was also estimated.
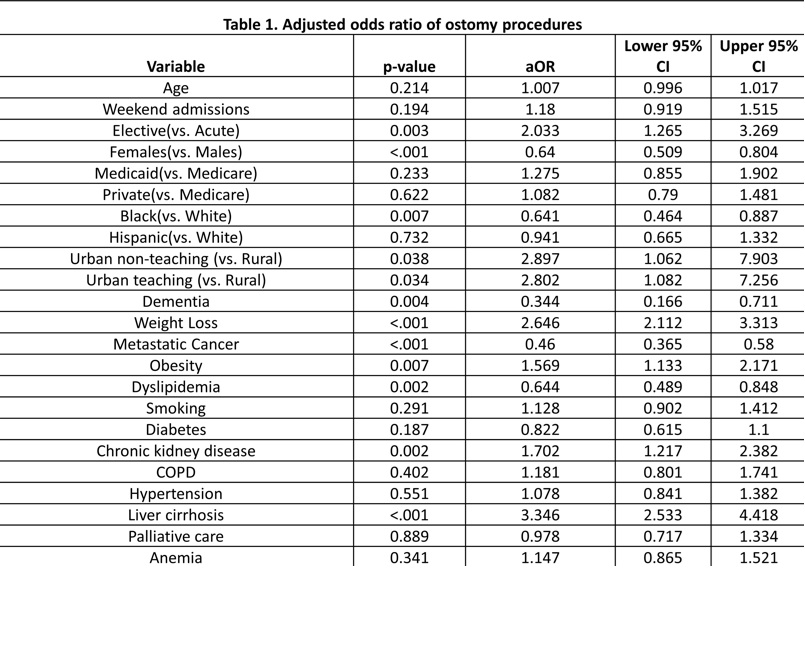
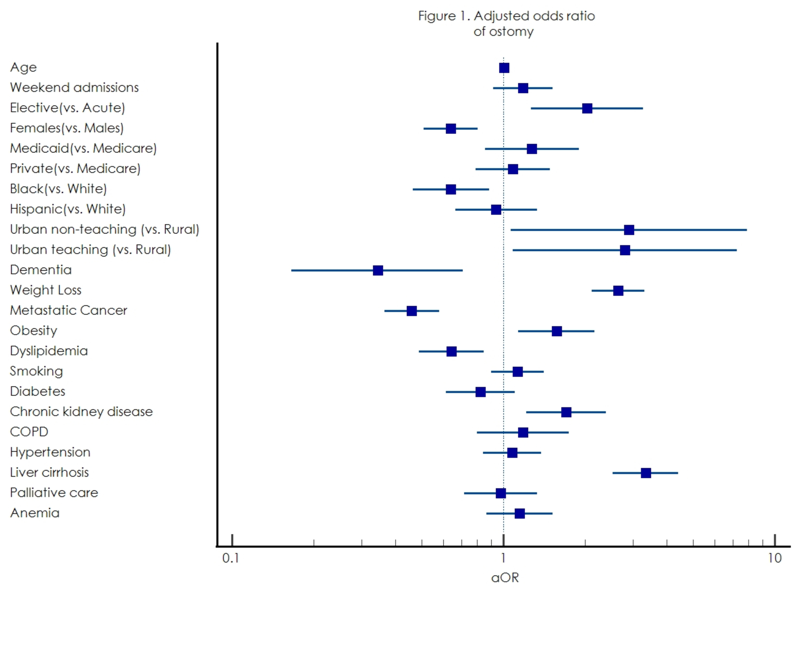
Results:
We identified 3555 cases of colon cancer who underwent colonic stenting between 2016 and
2021. The mean age of the sample was 65.0 years. Approximately 12.8%(455 cases) required ostomy
procedures. Further analysis found that patients who were hospitalized on an elective basis, treated at
urban teaching or non-teaching centers(vs. rural), had suffered weight loss or were diagnosed with obesity,
or had a history of chronic kidney disease, or liver cirrhosis, were more likely to undergo ostomy
procedures. Meanwhile, females(vs. males), patients with dementia, dyslipidemia, racially classified as
Blacks(vs. Whites), or with metastasis had lower odds of such procedures. No discrepancies were seen
based on their insurance form and other comorbidities, as illustrated in Table 1 and Figure 1. The need for
ostomy resulted in longer hospitalizations (mean stay of 15.52 days vs. 7.35, p< 0.01), with higher hospital
charges($240559 vs. $90496, p< 0.01). Around 11.0%(vs. 3.2%) of ostomy patients did not survive, which
affected an older group (mean age 71.20 vs. 65.57 years, p< 0.01), with a higher mean Charlson
Comorbidity Index(CCI) score (5.80 vs. 4.94, p=0.017).
Discussion:
Colon cancer patients undergoing colonic stenting for obstruction may require ostomy that can
be influenced by the sex of the patients, the location of the hospital, and various comorbidities. Ostomy in
older patients who are sicker may also lead to poorer outcomes. Therefore, physicians must conduct
meticulous pre-operative screening and adopt thorough post- operative follow-ups during their stay.
Disclosures:
Renuka Verma, MD1, Tejas Joshi, MD2, Kamleshun Ramphul, MD3, Krish Pandya, 4, Ahmed Sherif, MD2, Wesam Frandah, MD2. P4582 - Predictors of Ostomy and Outcomes in Colonic Stenting for Obstructing Colon Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
