Monday Poster Session
Category: IBD
P3277 - Prevalence of Clostridioides difficile Infection (CDI) and Mortality Predictors Among Inflammatory Bowel Disease (IBD) Patients in Comparison to Non-IBD Patients: A Nationwide Database Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Has Audio

Chloe Lahoud, MD
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Chloe Lahoud, MD1, Bivin George, DO, PharmD2, Chapman Wei, MD1, Liliane Deeb, MD1
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Staten Island University Hospital, Northwell Health, New York City, NY
Introduction: Inflammatory Bowel Disease (IBD) is characterized by chronic relapsing & remitting inflammation of the gastrointestinal tract. Clostridioides Difficile Infection (CDI) is the leading cause of colitis and hospital-acquired-diarrhea. The literature suggests IBD patients have worse outcomes when affected with CDI. This study aims to assess the prevalence and morality predictors of CDI in IBD.
Methods: Data for hospitalized patients with IBD was obtained from The National Inpatient Sample (NIS) database from 2016-2020. Patients were initially stratified into IBD and non-IBD groups, then into Crohn’s Disease (CD) and Ulcerative Colitis (UC) groups within IBD. Primary outcomes were prevalence and risk factors of CDI. Secondary outcomes were mortality and length of stay (LOS).
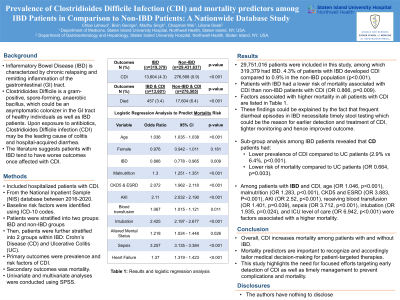
Results: 29,751,016 patients were included in this study, 319,379 had IBD. 4.3% of patients with IBD developed CDI compared to 0.9% in the non-IBD patients (p< 0.001). Overall, age (OR 1.036), malnutrition (OR 1.3), chronic kidney disease stage 5 (CKD5) and end stage renal disease (ESRD) (OR 2.07), acute kidney injury (AKI) (OR 2.1), receiving blood transfusion (OR 1.07), intubation (OR 2.43), sepsis (OR 3.26) and ICU level of care (OR 3.71) are associated with higher mortality in patients with CDI (p< 0.001). IBD patients with CDI had a lower risk of mortality than non-IBD patients with CDI (OR 0.87, p=0.009).
IBD sub-group analysis revealed 6.4% of UC patients developed CDI compared to 2.9% of CD patients (p< 0.001). Age (OR 1.05), malnutrition (OR 1.29), heart failure (OR 1.46), CKD5 and ESRD (OR 3.88), AKI (OR 2.52), sepsis (OR 3.71), intubation (OR 1.94), and ICU level of care (OR 6.94) were factors associated with a higher mortality (p< 0.001). CD patients had lower risk of mortality than UC patients (OR 0.66, p=0.003).
Discussion: IBD patients are at an increased risk of getting CDI but have a lower risk of mortality than those without IBD. These findings could be explained by frequent diarrheal episodes in IBD necessitating timely stool testing and earlier detection and treatment of CDI and tighter monitoring. Among IBD patients, both the incidence of CDI and related mortality were higher in patients with UC than CD. Mortality was much higher in IBD patients with CDI who required ICU care, compared to non-IBD counterparts (OR 6.9 vs 3.7, p< 0.001). This study highlights the need for efforts targeting early detection of CDI in IBD to tailor medical decision-making, prevent complications and improve patient outcomes.
Disclosures:
Chloe Lahoud, MD1, Bivin George, DO, PharmD2, Chapman Wei, MD1, Liliane Deeb, MD1. P3277 - Prevalence of <i>Clostridioides Difficile</i> Infection (CDI) and Mortality Predictors Among Inflammatory Bowel Disease (IBD) Patients in Comparison to Non-IBD Patients: A Nationwide Database Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Staten Island University Hospital, Northwell Health, New York City, NY
Introduction: Inflammatory Bowel Disease (IBD) is characterized by chronic relapsing & remitting inflammation of the gastrointestinal tract. Clostridioides Difficile Infection (CDI) is the leading cause of colitis and hospital-acquired-diarrhea. The literature suggests IBD patients have worse outcomes when affected with CDI. This study aims to assess the prevalence and morality predictors of CDI in IBD.
Methods: Data for hospitalized patients with IBD was obtained from The National Inpatient Sample (NIS) database from 2016-2020. Patients were initially stratified into IBD and non-IBD groups, then into Crohn’s Disease (CD) and Ulcerative Colitis (UC) groups within IBD. Primary outcomes were prevalence and risk factors of CDI. Secondary outcomes were mortality and length of stay (LOS).
Results: 29,751,016 patients were included in this study, 319,379 had IBD. 4.3% of patients with IBD developed CDI compared to 0.9% in the non-IBD patients (p< 0.001). Overall, age (OR 1.036), malnutrition (OR 1.3), chronic kidney disease stage 5 (CKD5) and end stage renal disease (ESRD) (OR 2.07), acute kidney injury (AKI) (OR 2.1), receiving blood transfusion (OR 1.07), intubation (OR 2.43), sepsis (OR 3.26) and ICU level of care (OR 3.71) are associated with higher mortality in patients with CDI (p< 0.001). IBD patients with CDI had a lower risk of mortality than non-IBD patients with CDI (OR 0.87, p=0.009).
IBD sub-group analysis revealed 6.4% of UC patients developed CDI compared to 2.9% of CD patients (p< 0.001). Age (OR 1.05), malnutrition (OR 1.29), heart failure (OR 1.46), CKD5 and ESRD (OR 3.88), AKI (OR 2.52), sepsis (OR 3.71), intubation (OR 1.94), and ICU level of care (OR 6.94) were factors associated with a higher mortality (p< 0.001). CD patients had lower risk of mortality than UC patients (OR 0.66, p=0.003).
Discussion: IBD patients are at an increased risk of getting CDI but have a lower risk of mortality than those without IBD. These findings could be explained by frequent diarrheal episodes in IBD necessitating timely stool testing and earlier detection and treatment of CDI and tighter monitoring. Among IBD patients, both the incidence of CDI and related mortality were higher in patients with UC than CD. Mortality was much higher in IBD patients with CDI who required ICU care, compared to non-IBD counterparts (OR 6.9 vs 3.7, p< 0.001). This study highlights the need for efforts targeting early detection of CDI in IBD to tailor medical decision-making, prevent complications and improve patient outcomes.
Disclosures:
Chloe Lahoud indicated no relevant financial relationships.
Bivin George indicated no relevant financial relationships.
Chapman Wei indicated no relevant financial relationships.
Liliane Deeb indicated no relevant financial relationships.
Chloe Lahoud, MD1, Bivin George, DO, PharmD2, Chapman Wei, MD1, Liliane Deeb, MD1. P3277 - Prevalence of <i>Clostridioides Difficile</i> Infection (CDI) and Mortality Predictors Among Inflammatory Bowel Disease (IBD) Patients in Comparison to Non-IBD Patients: A Nationwide Database Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
