Monday Poster Session
Category: Infections and Microbiome
P3428 - Comparative Efficacy of Tailored and Concomitant Therapy as First-Line Treatment for H. pylori: A Systematic Review and Meta-Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Has Audio
- MC
Muhammad YN Chaudhary, MBChB
Indiana University Southwest Internal Medicine Residency Program
Evansville, IN
Presenting Author(s)
Muhammad YN. Chaudhary, MBChB1, Mohammad Jawwad, MBBS2, Ayan Khalid, MBBS2, Anas Rasool, MBBS2, Sabula Tabish, MBBS2, Hafiz Muhammad Faizan. Abid, MBBS2, Shaikh Muhammad Daniyal, MBBS2, Isbah Gul, MBBS2, Oluwagbenga Serrano, MD, FACG3
1Indiana University Southwest Internal Medicine Residency Program, Evansville, IN; 2Dow Medical College, Karachi, Sindh, Pakistan; 3Indiana University School of Medicine, Vincennes, IN
Introduction: Rising antibiotic resistance has prompted interest in susceptibility-guided tailored therapy as an alternative to standard empirical regimens for Helicobacter pylori (H. pylori) eradication. While concomitant therapy is a widely used empirical approach, the comparative efficacy and safety of tailored therapy versus concomitant therapy as first-line treatment remain uncertain. We performed a meta‐analysis of randomised controlled trials (RCTs) comparing tailored versus concomitant therapy in patients with H. pylori infection.
Methods: We conducted a comprehensive literature search of PubMed, ScienceDirect, Cochrane CENTRAL, clinicaltrials.gov, and Google Scholar through May 2025 to identify studies comparing tailored therapy versus concomitant therapy for H. pylori eradication. Studies were included if they enrolled patients with confirmed H. pylori infection and reported at least one of the following outcomes: intention-to-treat (ITT) eradication rate, per-protocol (PP) eradication rate, compliance, or adverse events. Pooled risk ratios (RRs) and 95% confidence intervals (CIs) were calculated using a random-effects model. Heterogeneity was assessed using the I² statistic, and all analyses were performed using Review Manager 5.4.
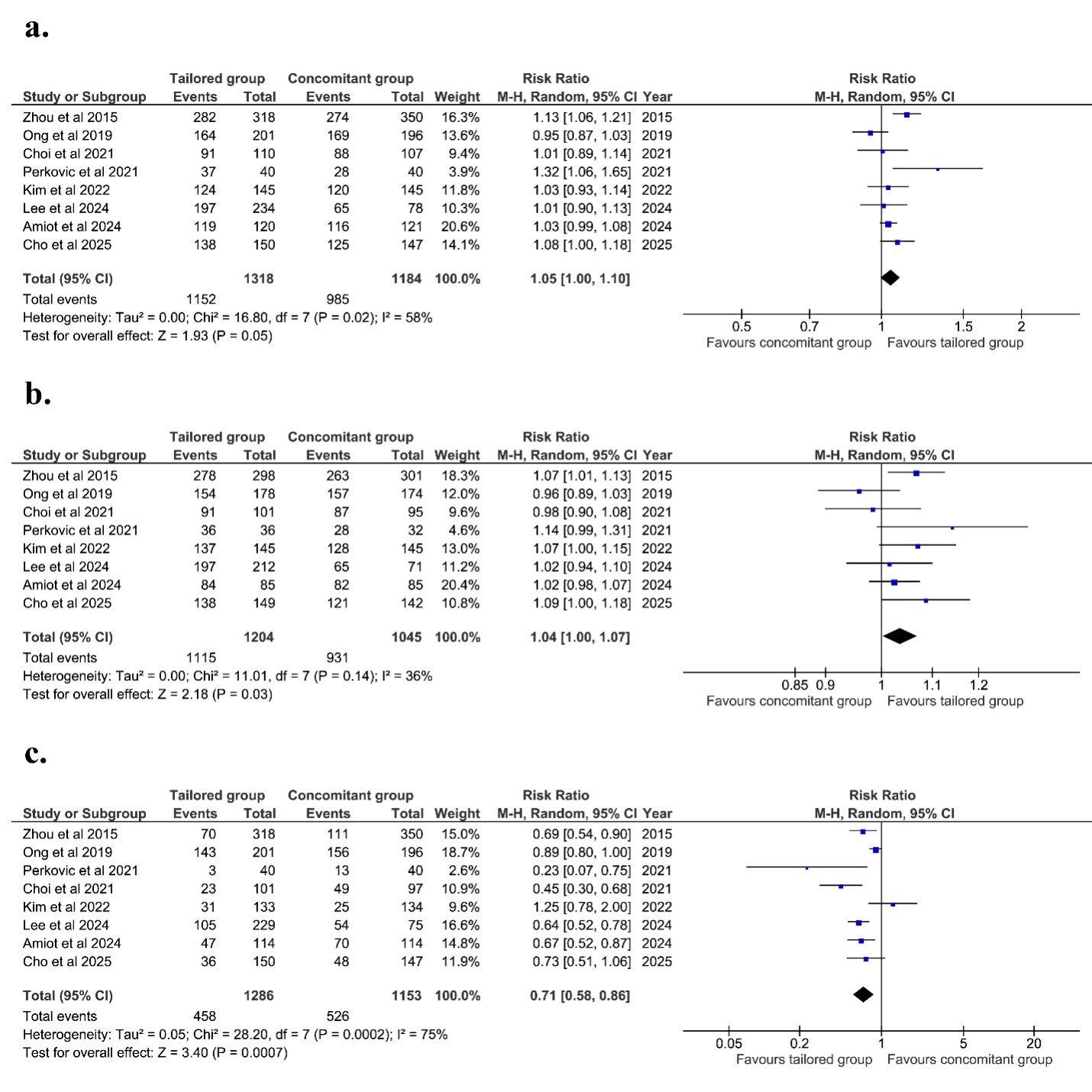
Results: Eight RCTs (n = 2,534; 1,374 assigned to tailored therapy and 1,208 assigned to concomitant therapy) met the eligibility criteria. The eradication rates were significantly higher in the tailored group than in the concomitant group in both the ITT analysis (87.4% vs. 83.2%; RR 1.05; [95% CI: 1.00 to 1.10]; p = 0.05) and PP analysis (92.6% vs. 89.1%, RR 1.04; [95% CI: 1.00 to 1.07]; p = 0.03). Adverse events occurred less frequently with tailored therapy than with concomitant therapy (35.6% vs. 45.6%; RR 0.71; [95% CI 0.58 to 0.86]; p = 0.0007). Figure 1 summarises the results.
Discussion: We found that tailored therapy was associated with higher eradication rates and fewer adverse events compared to concomitant therapy. These findings suggest that tailored therapy provides a more effective option for H. pylori eradication, especially in settings with antibiotic resistance.
Disclosures:
Muhammad YN. Chaudhary, MBChB1, Mohammad Jawwad, MBBS2, Ayan Khalid, MBBS2, Anas Rasool, MBBS2, Sabula Tabish, MBBS2, Hafiz Muhammad Faizan. Abid, MBBS2, Shaikh Muhammad Daniyal, MBBS2, Isbah Gul, MBBS2, Oluwagbenga Serrano, MD, FACG3. P3428 - Comparative Efficacy of Tailored and Concomitant Therapy as First-Line Treatment for <i>H. pylori</i>: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Indiana University Southwest Internal Medicine Residency Program, Evansville, IN; 2Dow Medical College, Karachi, Sindh, Pakistan; 3Indiana University School of Medicine, Vincennes, IN
Introduction: Rising antibiotic resistance has prompted interest in susceptibility-guided tailored therapy as an alternative to standard empirical regimens for Helicobacter pylori (H. pylori) eradication. While concomitant therapy is a widely used empirical approach, the comparative efficacy and safety of tailored therapy versus concomitant therapy as first-line treatment remain uncertain. We performed a meta‐analysis of randomised controlled trials (RCTs) comparing tailored versus concomitant therapy in patients with H. pylori infection.
Methods: We conducted a comprehensive literature search of PubMed, ScienceDirect, Cochrane CENTRAL, clinicaltrials.gov, and Google Scholar through May 2025 to identify studies comparing tailored therapy versus concomitant therapy for H. pylori eradication. Studies were included if they enrolled patients with confirmed H. pylori infection and reported at least one of the following outcomes: intention-to-treat (ITT) eradication rate, per-protocol (PP) eradication rate, compliance, or adverse events. Pooled risk ratios (RRs) and 95% confidence intervals (CIs) were calculated using a random-effects model. Heterogeneity was assessed using the I² statistic, and all analyses were performed using Review Manager 5.4.
Results: Eight RCTs (n = 2,534; 1,374 assigned to tailored therapy and 1,208 assigned to concomitant therapy) met the eligibility criteria. The eradication rates were significantly higher in the tailored group than in the concomitant group in both the ITT analysis (87.4% vs. 83.2%; RR 1.05; [95% CI: 1.00 to 1.10]; p = 0.05) and PP analysis (92.6% vs. 89.1%, RR 1.04; [95% CI: 1.00 to 1.07]; p = 0.03). Adverse events occurred less frequently with tailored therapy than with concomitant therapy (35.6% vs. 45.6%; RR 0.71; [95% CI 0.58 to 0.86]; p = 0.0007). Figure 1 summarises the results.
Discussion: We found that tailored therapy was associated with higher eradication rates and fewer adverse events compared to concomitant therapy. These findings suggest that tailored therapy provides a more effective option for H. pylori eradication, especially in settings with antibiotic resistance.
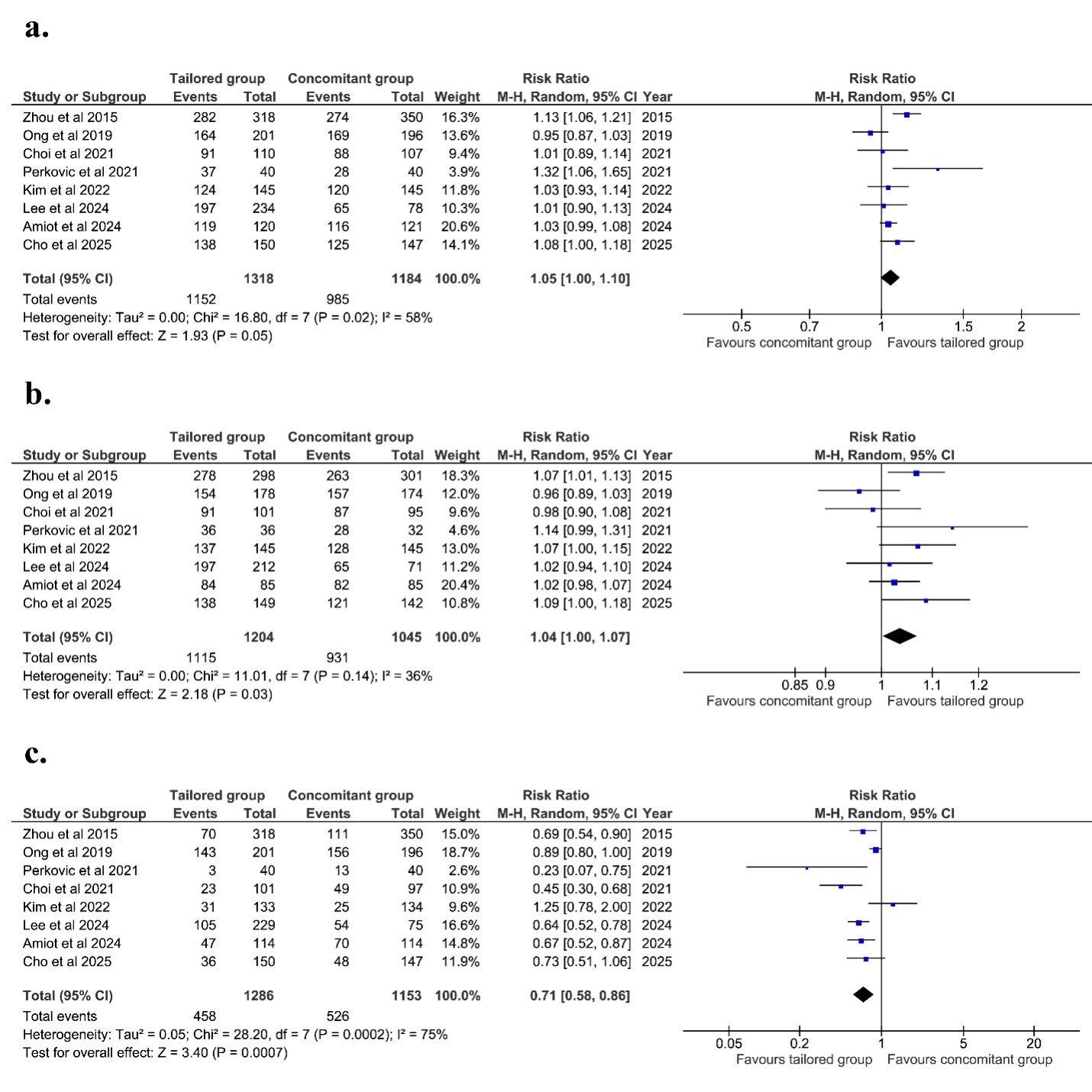
Figure: Figure 1: Forest plots of the eradication rates with intention-to-treat (a) and per-protocol (b) analysis and (c) adverse events.
Disclosures:
Muhammad Chaudhary indicated no relevant financial relationships.
Mohammad Jawwad indicated no relevant financial relationships.
Ayan Khalid indicated no relevant financial relationships.
Anas Rasool indicated no relevant financial relationships.
Sabula Tabish indicated no relevant financial relationships.
Hafiz Muhammad Abid indicated no relevant financial relationships.
Shaikh Muhammad Daniyal indicated no relevant financial relationships.
Isbah Gul indicated no relevant financial relationships.
Oluwagbenga Serrano indicated no relevant financial relationships.
Muhammad YN. Chaudhary, MBChB1, Mohammad Jawwad, MBBS2, Ayan Khalid, MBBS2, Anas Rasool, MBBS2, Sabula Tabish, MBBS2, Hafiz Muhammad Faizan. Abid, MBBS2, Shaikh Muhammad Daniyal, MBBS2, Isbah Gul, MBBS2, Oluwagbenga Serrano, MD, FACG3. P3428 - Comparative Efficacy of Tailored and Concomitant Therapy as First-Line Treatment for <i>H. pylori</i>: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
