Monday Poster Session
Category: Infections and Microbiome
P3438 - Predictors of Clostridioides difficile Infection in Hospitalized Patients With End-Stage Renal Disease: Insights from a Large Cohort Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Has Audio

Joelle Sleiman, MD
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Joelle Sleiman, MD1, Taimur Aslam, MD1, Un Jung Lee, PhD2, Ryan Njeim, MD1, Suzanne El-Sayegh, MD1, Liliane Deeb, MD1
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Biostatics Unit, Office of Academic Affairs, Northwell Health, Staten Island, NY
Introduction: Clostridioides difficile infection (CDI) is a serious infection with increased morbidity and mortality. Patients with end-stage renal disease (ESRD) are at increased risk of developing CDI compared to the general population. We aim to assess the predictors of developing CDI specifically for this high-risk population.
Methods: Using the Northwell HIE database from 2018 to 2021, we included a total of 11,259 hospitalized patients with end-stage renal disease. Demographics and clinical variables were collected. The primary endpoint was the development of Clostridioides difficile infection. Univariate analysis was performed to assess the association between the primary endpoint and each risk factor. Logistic regression adjusting for gender, age group, BMI group, and race was performed for each risk factor in separate models. All statistical tests were two-sided at a significance level of 0.05.
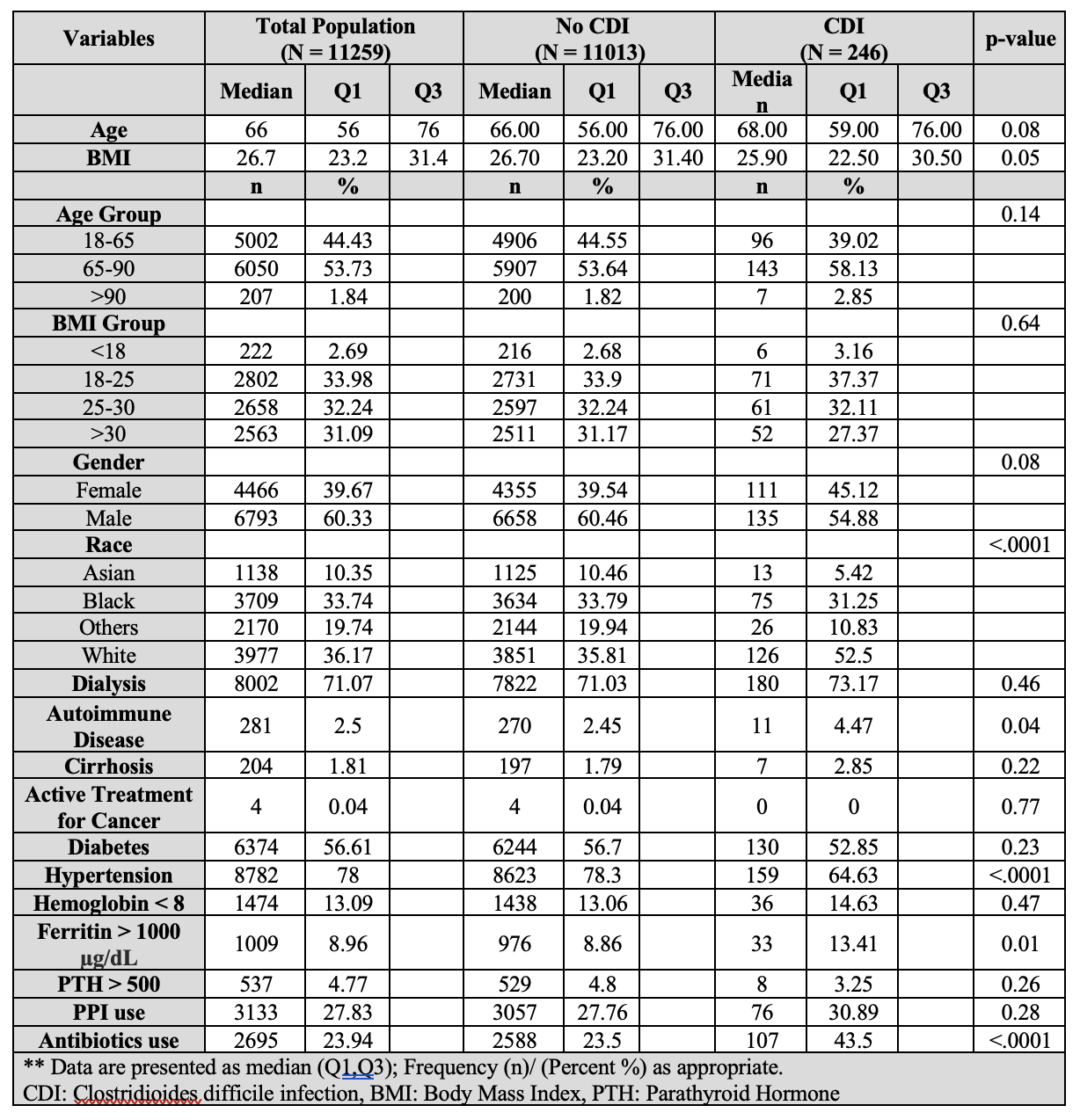
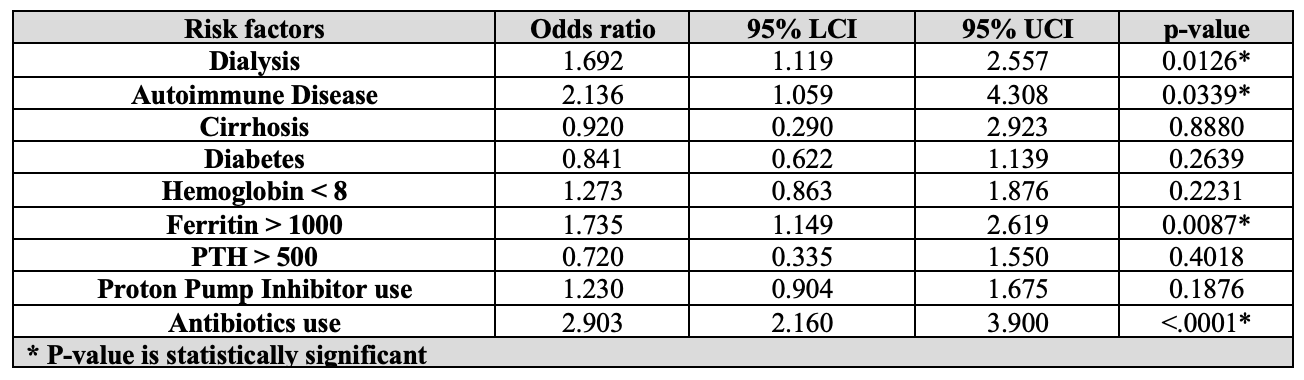
Results: Of 11,259 hospitalized patients with ESRD (aged 65.1 ± 14.7 years; 60.3% male; 36.2% white), 246 (2.2%) developed CDI, while 11,013 (97.8%) did not (Table 1). Univariate analysis identified several significant risk factors for CDI. Patients with autoimmune diseases were 86% more likely to develop CDI (OR: 1.86, 95% CI: 1.00–3.45). Patients with ferritin levels greater than 1000 µg/dL were 59% more likely to develop CDI (OR: 1.59, 95% CI: 1.10–2.29). Antibiotic use increased CDI risk by 149% (OR: 2.49, 95% CI: 1.93–3.21). Logistic regression analyses adjusting for gender, age group, BMI group, and race, identified significant predictors: dialysis, autoimmune disease, high ferritin levels, and antibiotic use. Dialysis increased CDI risk by 69% (OR: 1.69, 95% CI: 1.12–2.56). High ferritin levels ( >1000) increased CDI risk by 74% (OR: 1.735, 95% CI: 1.149-2.619). Autoimmune disease doubled the risk of developing CDI (OR: 2.136, 95% CI: 1.059-4.308). Antibiotic use nearly tripled CDI risk (OR: 2.90, 95% CI: 2.16–3.90) (Table 2).
Discussion: We identified several significant predictors of Clostridioides difficile infection in hospitalized patients with end-stage renal disease, including dialysis, autoimmune disease, elevated ferritin levels, and antibiotic use. These findings emphasize the need for targeted risk mitigation strategies in patients with ESRD, particularly when they have high-risk clinical profiles.
Disclosures:
Joelle Sleiman, MD1, Taimur Aslam, MD1, Un Jung Lee, PhD2, Ryan Njeim, MD1, Suzanne El-Sayegh, MD1, Liliane Deeb, MD1. P3438 - Predictors of <i>Clostridioides Difficile</i> Infection in Hospitalized Patients With End-Stage Renal Disease: Insights from a Large Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Biostatics Unit, Office of Academic Affairs, Northwell Health, Staten Island, NY
Introduction: Clostridioides difficile infection (CDI) is a serious infection with increased morbidity and mortality. Patients with end-stage renal disease (ESRD) are at increased risk of developing CDI compared to the general population. We aim to assess the predictors of developing CDI specifically for this high-risk population.
Methods: Using the Northwell HIE database from 2018 to 2021, we included a total of 11,259 hospitalized patients with end-stage renal disease. Demographics and clinical variables were collected. The primary endpoint was the development of Clostridioides difficile infection. Univariate analysis was performed to assess the association between the primary endpoint and each risk factor. Logistic regression adjusting for gender, age group, BMI group, and race was performed for each risk factor in separate models. All statistical tests were two-sided at a significance level of 0.05.
Results: Of 11,259 hospitalized patients with ESRD (aged 65.1 ± 14.7 years; 60.3% male; 36.2% white), 246 (2.2%) developed CDI, while 11,013 (97.8%) did not (Table 1). Univariate analysis identified several significant risk factors for CDI. Patients with autoimmune diseases were 86% more likely to develop CDI (OR: 1.86, 95% CI: 1.00–3.45). Patients with ferritin levels greater than 1000 µg/dL were 59% more likely to develop CDI (OR: 1.59, 95% CI: 1.10–2.29). Antibiotic use increased CDI risk by 149% (OR: 2.49, 95% CI: 1.93–3.21). Logistic regression analyses adjusting for gender, age group, BMI group, and race, identified significant predictors: dialysis, autoimmune disease, high ferritin levels, and antibiotic use. Dialysis increased CDI risk by 69% (OR: 1.69, 95% CI: 1.12–2.56). High ferritin levels ( >1000) increased CDI risk by 74% (OR: 1.735, 95% CI: 1.149-2.619). Autoimmune disease doubled the risk of developing CDI (OR: 2.136, 95% CI: 1.059-4.308). Antibiotic use nearly tripled CDI risk (OR: 2.90, 95% CI: 2.16–3.90) (Table 2).
Discussion: We identified several significant predictors of Clostridioides difficile infection in hospitalized patients with end-stage renal disease, including dialysis, autoimmune disease, elevated ferritin levels, and antibiotic use. These findings emphasize the need for targeted risk mitigation strategies in patients with ESRD, particularly when they have high-risk clinical profiles.
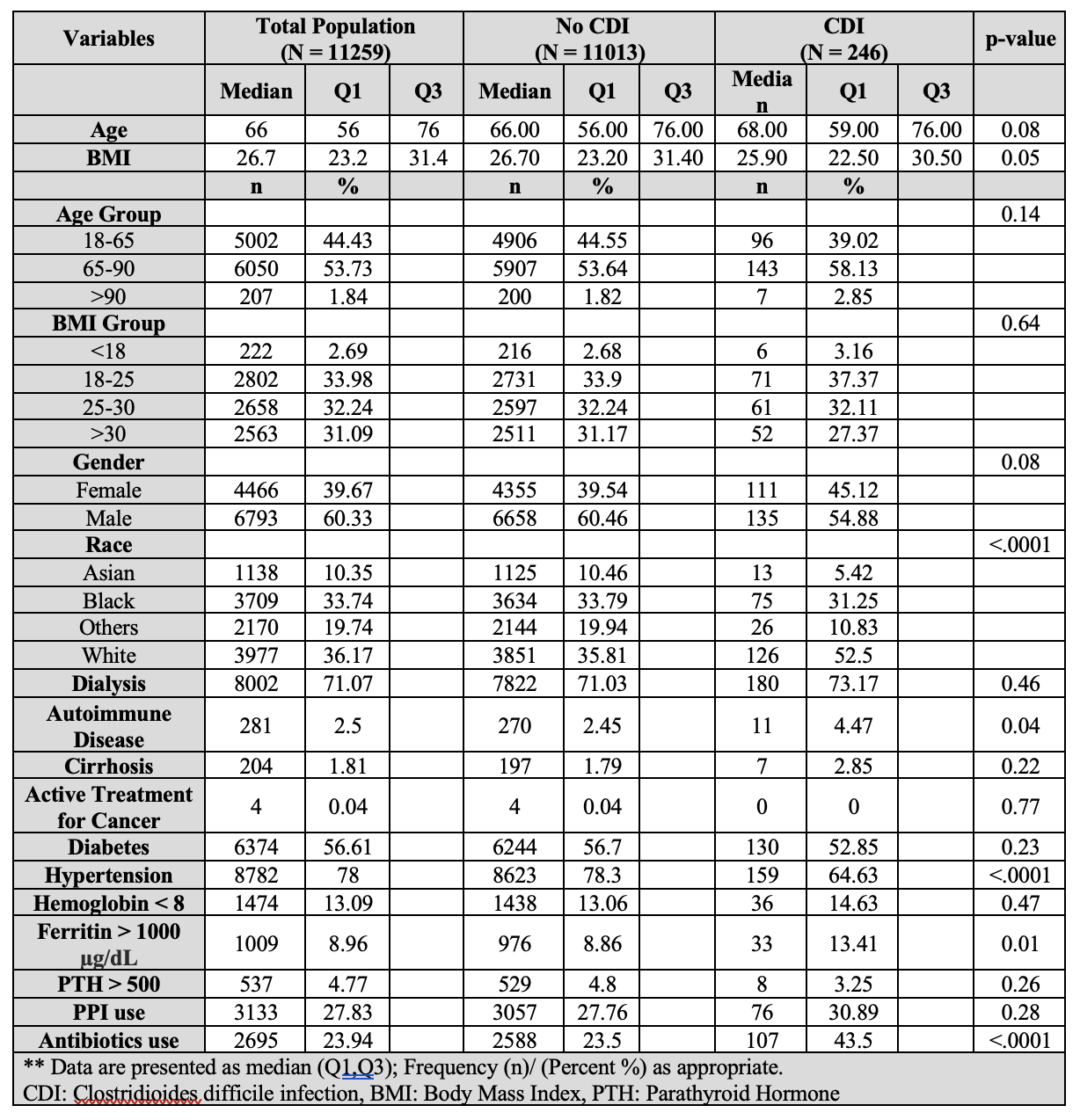
Figure: Table 1. Demographic and Clinical Characteristics
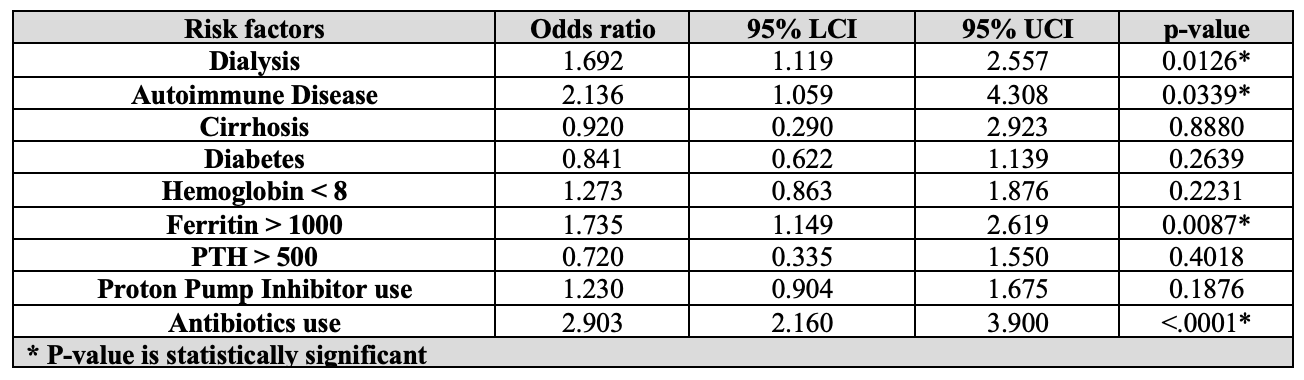
Figure: Table 2. Logistic Regression results for each risk factor, adjusting for gender, age group, BMI group, and race.
Disclosures:
Joelle Sleiman indicated no relevant financial relationships.
Taimur Aslam indicated no relevant financial relationships.
Un Jung Lee indicated no relevant financial relationships.
Ryan Njeim indicated no relevant financial relationships.
Suzanne El-Sayegh indicated no relevant financial relationships.
Liliane Deeb indicated no relevant financial relationships.
Joelle Sleiman, MD1, Taimur Aslam, MD1, Un Jung Lee, PhD2, Ryan Njeim, MD1, Suzanne El-Sayegh, MD1, Liliane Deeb, MD1. P3438 - Predictors of <i>Clostridioides Difficile</i> Infection in Hospitalized Patients With End-Stage Renal Disease: Insights from a Large Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
