Monday Poster Session
Category: Infections and Microbiome
P3460 - Mesenteric Venous Ischemia Due to Splanchnic Venous Thrombosis in a Case of Clostridioides difficile Colitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Has Audio

Prashanth Kotla, BA
John Sealy School of Medicine, University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Prashanth Kotla, BA1, Hari Movva, MD2, Edward Butt, MD, MPH2, Sreeram Parupudi, MD2
1John Sealy School of Medicine, University of Texas Medical Branch, Galveston, TX; 2University of Texas Medical Branch, Galveston, TX
Introduction: Clostridioides difficile (C. diff) colitis is a rare but potential cause of venous thromboembolism (VTE), including in the splanchnic circulation. Few such cases are reported, and the pathophysiology may involve sepsis-related endothelial dysfunction, systemic inflammation, and hypercoagulability. We report a case of splanchnic venous thrombosis in a patient with C. diff colitis.
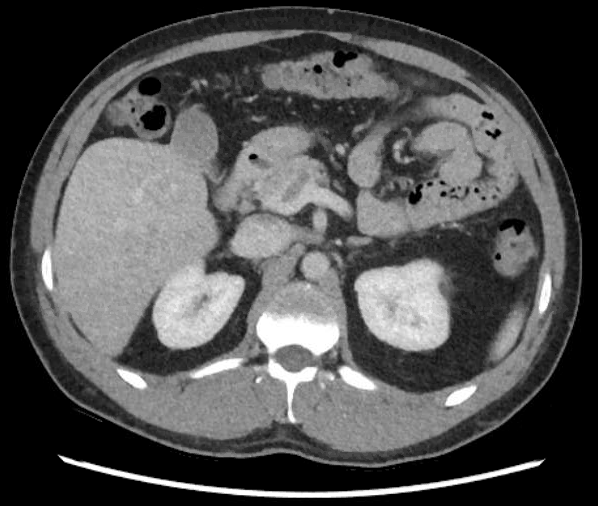
Case Description/Methods: A 43-year-old male with hypertension presented to the emergency room (ER) with abdominal pain. Two weeks prior, he was treated for presumed diverticulitis at urgent care with amoxicillin-clavulanate but noted worsening symptoms. On the day of admission, a CT abdomen/pelvis from another urgent care showed terminal ileitis, raising concern for Crohn’s disease. ER labs revealed leukocytosis (WBC: 15.48 × 10⁹/L), elevated liver enzymes (ALP: 135 U/L, ALT: 82 U/L, AST: 84 U/L), and a positive C. diff toxin test. Subsequent lactate was normal (1.39 mm/L). CT angiogram showed thrombosis in the posterior right portal vein branch, distal main portal vein, and superior mesenteric vein and its distal branches with signs of potential small bowel venous infarction seen as increased bowel wall thickening and surrounding fat stranding of ileal loops in the right upper quadrant distal to the venous occlusion (Figure 1 and 2). The patient began a 10-day course of vancomycin and apixaban with symptomatic improvement. No vascular intervention was pursued. He was discharged on the same regimen. At follow-up, CT angiogram showed improving thrombosis and small bowel inflammation. A hypercoagulability panel was unremarkable, and outpatient colonoscopy did not support Crohn’s disease, suggesting the ileitis was due to venous infarction.
Discussion: Diverticulitis may lead to septic thrombosis (pylephlebitis) of the portal vein or its tributaries via inflammation-mediated clot formation, but the event rate of pylephlebitis in abdominal infection is low. The potential contribution of a recent episode of diverticulitis to thrombus formation warrants further investigation. While C. diff colitis is not a common cause of VTE, a multifactorial interplay, particularly sepsis-induced hypercoagulability, may contribute to thrombosis. A retrospective study of surgical ICU patients by Barmparas et al. showed almost twice the chance of VTE formation in C. diff positive versus negative patients (p = 0.049). Abdominal deep vein thromboses should be considered in the setting of C. diff colitis given risks in morbidity and mortality.

Disclosures:
Prashanth Kotla, BA1, Hari Movva, MD2, Edward Butt, MD, MPH2, Sreeram Parupudi, MD2. P3460 - Mesenteric Venous Ischemia Due to Splanchnic Venous Thrombosis in a Case of <i>Clostridioides difficile</i> Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1John Sealy School of Medicine, University of Texas Medical Branch, Galveston, TX; 2University of Texas Medical Branch, Galveston, TX
Introduction: Clostridioides difficile (C. diff) colitis is a rare but potential cause of venous thromboembolism (VTE), including in the splanchnic circulation. Few such cases are reported, and the pathophysiology may involve sepsis-related endothelial dysfunction, systemic inflammation, and hypercoagulability. We report a case of splanchnic venous thrombosis in a patient with C. diff colitis.
Case Description/Methods: A 43-year-old male with hypertension presented to the emergency room (ER) with abdominal pain. Two weeks prior, he was treated for presumed diverticulitis at urgent care with amoxicillin-clavulanate but noted worsening symptoms. On the day of admission, a CT abdomen/pelvis from another urgent care showed terminal ileitis, raising concern for Crohn’s disease. ER labs revealed leukocytosis (WBC: 15.48 × 10⁹/L), elevated liver enzymes (ALP: 135 U/L, ALT: 82 U/L, AST: 84 U/L), and a positive C. diff toxin test. Subsequent lactate was normal (1.39 mm/L). CT angiogram showed thrombosis in the posterior right portal vein branch, distal main portal vein, and superior mesenteric vein and its distal branches with signs of potential small bowel venous infarction seen as increased bowel wall thickening and surrounding fat stranding of ileal loops in the right upper quadrant distal to the venous occlusion (Figure 1 and 2). The patient began a 10-day course of vancomycin and apixaban with symptomatic improvement. No vascular intervention was pursued. He was discharged on the same regimen. At follow-up, CT angiogram showed improving thrombosis and small bowel inflammation. A hypercoagulability panel was unremarkable, and outpatient colonoscopy did not support Crohn’s disease, suggesting the ileitis was due to venous infarction.
Discussion: Diverticulitis may lead to septic thrombosis (pylephlebitis) of the portal vein or its tributaries via inflammation-mediated clot formation, but the event rate of pylephlebitis in abdominal infection is low. The potential contribution of a recent episode of diverticulitis to thrombus formation warrants further investigation. While C. diff colitis is not a common cause of VTE, a multifactorial interplay, particularly sepsis-induced hypercoagulability, may contribute to thrombosis. A retrospective study of surgical ICU patients by Barmparas et al. showed almost twice the chance of VTE formation in C. diff positive versus negative patients (p = 0.049). Abdominal deep vein thromboses should be considered in the setting of C. diff colitis given risks in morbidity and mortality.
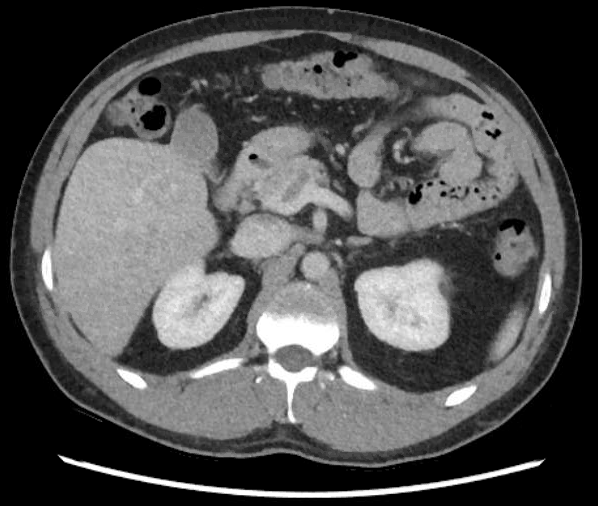
Figure: Figure 1: CT angiogram showing filling defects are noted again in the posterior right portal vein branch.

Figure: Figure 2: CT angiogram showing thrombus at the distal aspect of the main portal vein at the portal splenic confluence.
Disclosures:
Prashanth Kotla indicated no relevant financial relationships.
Hari Movva indicated no relevant financial relationships.
Edward Butt indicated no relevant financial relationships.
Sreeram Parupudi indicated no relevant financial relationships.
Prashanth Kotla, BA1, Hari Movva, MD2, Edward Butt, MD, MPH2, Sreeram Parupudi, MD2. P3460 - Mesenteric Venous Ischemia Due to Splanchnic Venous Thrombosis in a Case of <i>Clostridioides difficile</i> Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
