Monday Poster Session
Category: Infections and Microbiome
P3451 - The Colitis Conundrum: Recurrent C. difficile and CMV Colitis in a Patient With Underlying Ulcerative Colitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Has Audio

Amanda Renee Eukovich, DO
Broward Health Medical Center
Pompano Beach, FL
Presenting Author(s)
Amanda Renee. Eukovich, DO1, Lorraine Chong Tai, MD2, Ivana Rubenstein, DO2, Erik Aleman Espino, DO2, Edwin Makarevich, DO2, Andrea Escalante, DO2, Ronen Arai, MD3
1Broward Health Medical Center, Pompano Beach, FL; 2Broward Health Medical Center, Fort Lauderdale, FL; 3Gastro Health, Coral Springs, FL
Introduction: Ulcerative colitis (UC) is a chronic inflammatory condition with complex environmental and genetic influences, complicated by a dysregulated immune response and gut dysbiosis. Clostridium difficile (C. diff) is a toxin-mediated enterocolitis typically resulting from a deranged microbiome. Cytomegalovirus (CMV) is a ubiquitous herpesvirus that can lead to fulminant colitis in immunocompromised hosts.
Case Description/Methods: A 58-year old male with a history of recurrent C. diff colitis presented with hematochezia and tenesmus. Prior C. diff infections were resistant to vancomycin and metronidazole, only improving with fidaxomicin. On this hospitalization, the patient presented with a hemoglobin of 7.2g/dL, and a sigmoidoscopy revealed severe colitis. Histology demonstrated crypt abscesses consistent with active UC. Strikingly, biopsies also revealed superimposed CMV colitis, prompting treatment with both methylprednisolone and ganciclovir. A sigmoidoscopy three months later showed inflamed pseudopolyps. Biopsies confirmed active chronic inflammation with cryptitis, but CMV inclusion bodies were no longer found. He was treated for UC with infliximab but had persistent hematochezia. He was transitioned to Upadacitinib with improvement. One year later, he again developed C. diff colitis, leading to a UC flare. He was treated with Bezlotoxumab, but follow-up colonoscopy with biopsy showed pancolitis with CMV-infected cells. Alongside Upadacitinib, he started ganciclovir and fecal microbiota spore live-brpk capsules. After five months, a repeat colonoscopy finally showed significant mucosal healing.
Discussion: UC increases the risk of recurrent C. diff and CMV due to microbiome disturbance. UC patients often have increased colonic sulfate-reducing bacteria. Because of this, UC patients typically have gut dysbiosis with increased inflammatory expression, which impairs tight junctions and increases bacterial translocation. This patient had failed all other C. diff treatments in the past. He also failed UC treatment with infliximab. Oftentimes, patients with coinfections in UC require colectomy. Remarkably, the use of fecal live-brpk capsules to restore the microbiome, aggressive therapy with ganciclovir to treat CMV, and rescue therapy with Upadacitinib allowed the patient to reach clinical remission.
This case highlights the importance of revitalizing the microbiome in IBD patients to achieve remission. Until the microbiome was optimized, prior therapies targeting CMV and C. diff were ineffective.
Disclosures:
Amanda Renee. Eukovich, DO1, Lorraine Chong Tai, MD2, Ivana Rubenstein, DO2, Erik Aleman Espino, DO2, Edwin Makarevich, DO2, Andrea Escalante, DO2, Ronen Arai, MD3. P3451 - The Colitis Conundrum: Recurrent <i>C. difficile</i> and CMV Colitis in a Patient With Underlying Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Broward Health Medical Center, Pompano Beach, FL; 2Broward Health Medical Center, Fort Lauderdale, FL; 3Gastro Health, Coral Springs, FL
Introduction: Ulcerative colitis (UC) is a chronic inflammatory condition with complex environmental and genetic influences, complicated by a dysregulated immune response and gut dysbiosis. Clostridium difficile (C. diff) is a toxin-mediated enterocolitis typically resulting from a deranged microbiome. Cytomegalovirus (CMV) is a ubiquitous herpesvirus that can lead to fulminant colitis in immunocompromised hosts.
Case Description/Methods: A 58-year old male with a history of recurrent C. diff colitis presented with hematochezia and tenesmus. Prior C. diff infections were resistant to vancomycin and metronidazole, only improving with fidaxomicin. On this hospitalization, the patient presented with a hemoglobin of 7.2g/dL, and a sigmoidoscopy revealed severe colitis. Histology demonstrated crypt abscesses consistent with active UC. Strikingly, biopsies also revealed superimposed CMV colitis, prompting treatment with both methylprednisolone and ganciclovir. A sigmoidoscopy three months later showed inflamed pseudopolyps. Biopsies confirmed active chronic inflammation with cryptitis, but CMV inclusion bodies were no longer found. He was treated for UC with infliximab but had persistent hematochezia. He was transitioned to Upadacitinib with improvement. One year later, he again developed C. diff colitis, leading to a UC flare. He was treated with Bezlotoxumab, but follow-up colonoscopy with biopsy showed pancolitis with CMV-infected cells. Alongside Upadacitinib, he started ganciclovir and fecal microbiota spore live-brpk capsules. After five months, a repeat colonoscopy finally showed significant mucosal healing.
Discussion: UC increases the risk of recurrent C. diff and CMV due to microbiome disturbance. UC patients often have increased colonic sulfate-reducing bacteria. Because of this, UC patients typically have gut dysbiosis with increased inflammatory expression, which impairs tight junctions and increases bacterial translocation. This patient had failed all other C. diff treatments in the past. He also failed UC treatment with infliximab. Oftentimes, patients with coinfections in UC require colectomy. Remarkably, the use of fecal live-brpk capsules to restore the microbiome, aggressive therapy with ganciclovir to treat CMV, and rescue therapy with Upadacitinib allowed the patient to reach clinical remission.
This case highlights the importance of revitalizing the microbiome in IBD patients to achieve remission. Until the microbiome was optimized, prior therapies targeting CMV and C. diff were ineffective.
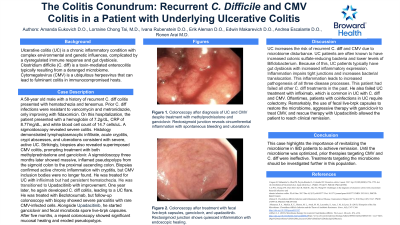
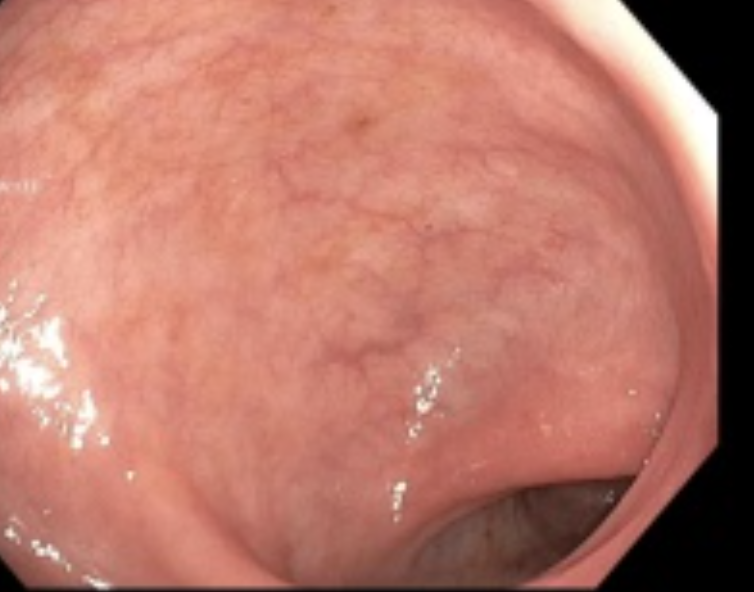
Figure: Figure 1. Colonoscopy after diagnosis of UC and CMV despite treatment with methylprednisolone and ganciclovir. Rectosigmoid junction reveals circumferential inflammation with spontaneous bleeding and ulcerations
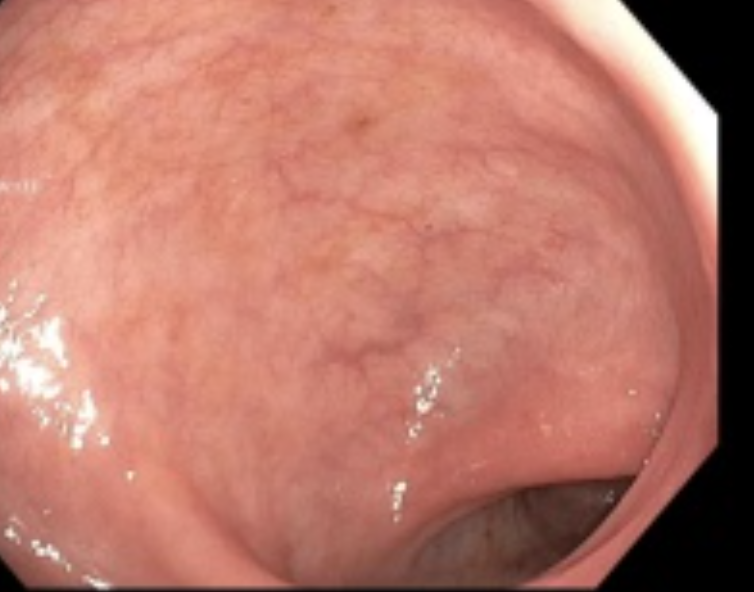
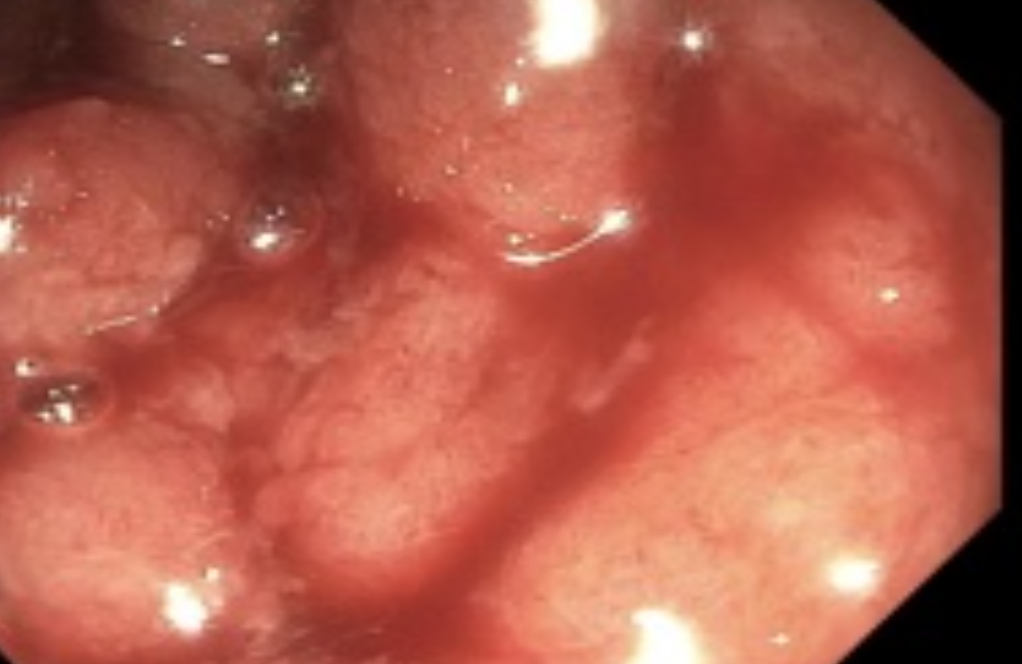
Figure: Figure 2. Colonoscopy after treatment with fecal live-brpk capsules, ganciclovir, and upadacitinib. Rectosigmoid junction shows quiesced inflammation with endoscopic healing.
Disclosures:
Amanda Eukovich indicated no relevant financial relationships.
Lorraine Chong Tai indicated no relevant financial relationships.
Ivana Rubenstein indicated no relevant financial relationships.
Erik Aleman Espino indicated no relevant financial relationships.
Edwin Makarevich indicated no relevant financial relationships.
Andrea Escalante indicated no relevant financial relationships.
Ronen Arai: Abbvie – Speakers Bureau. Castle Biosciences – Speakers Bureau. Celltrion – Speakers Bureau. Eli Lilly – Speakers Bureau. Johnson & Johnson – Speakers Bureau. Pfizer – Speakers Bureau. Phathom – Speakers Bureau.
Amanda Renee. Eukovich, DO1, Lorraine Chong Tai, MD2, Ivana Rubenstein, DO2, Erik Aleman Espino, DO2, Edwin Makarevich, DO2, Andrea Escalante, DO2, Ronen Arai, MD3. P3451 - The Colitis Conundrum: Recurrent <i>C. difficile</i> and CMV Colitis in a Patient With Underlying Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
