Monday Poster Session
Category: Colon
P2490 - Beyond the Adenoma: A Rare Case of Colonic Melanoma Metastasis
- DK
Diksha Kajal, MD
Florida State University
Cape Coral, FL
Presenting Author(s)
1Florida State University, Cape Coral, FL; 2North Central Bronx Hospital, Bronx, NY; 3Lee Health, Cape Coral, FL
Introduction:
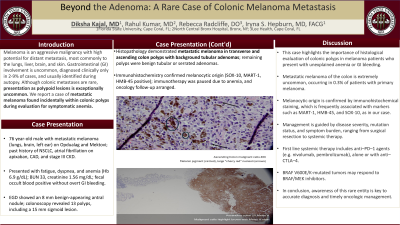
Melanoma is an aggressive malignancy with high potential for distant metastasis, most commonly to the lungs, liver, brain, and skin. Gastrointestinal (GI) involvement is uncommon, diagnosed clinically only in 2-9% of cases, and usually identified during autopsy. Although colonic metastases are rare, presentation as polypoid lesions is exceptionally uncommon. We report a case of metastatic melanoma found incidentally within colonic polyps during evaluation for symptomatic anemia.
Case Description/Methods:
A 76-year-old male with metastatic melanoma (lungs, brain, left ear) was receiving Opdualag and Mektovi. His history included non-small cell lung cancer, atrial fibrillation on apixaban, CAD, and stage III CKD. He presented with fatigue, dyspnea, and anemia (Hb 6.9 g/dL), with BUN 33 and creatinine 1.56 mg/dL. He denied GI bleeding, but fecal occult blood was positive.
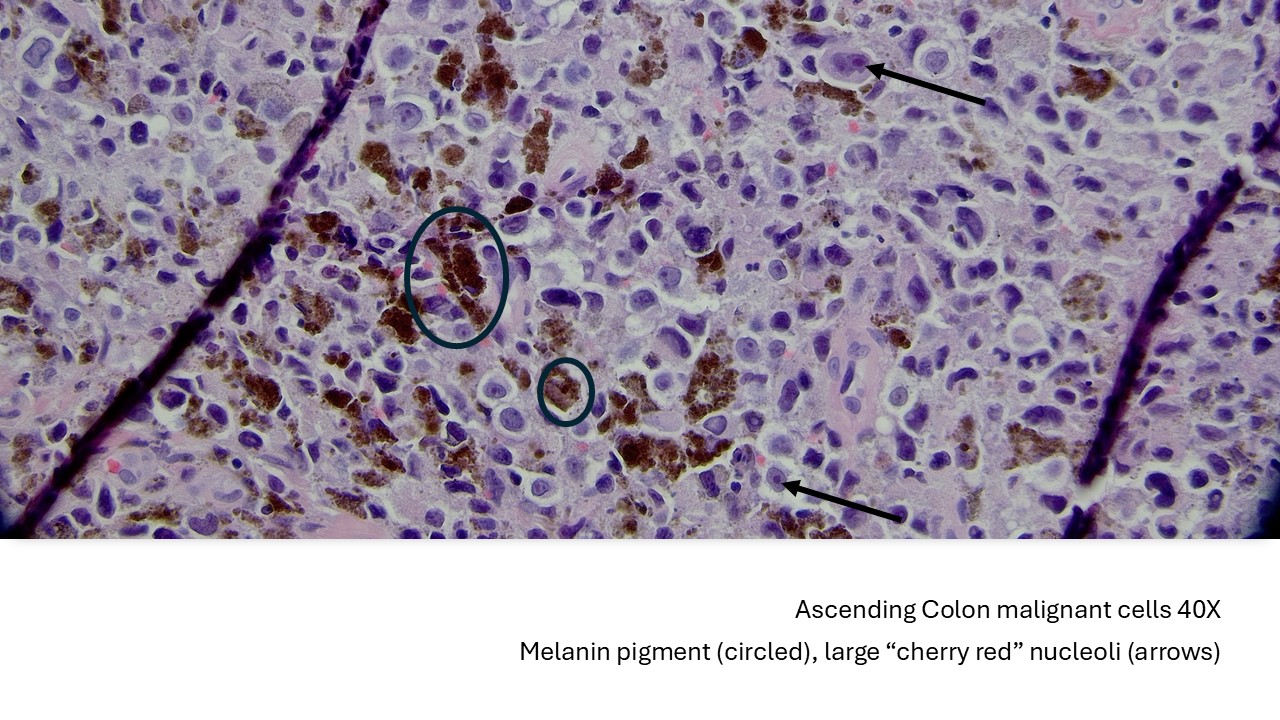
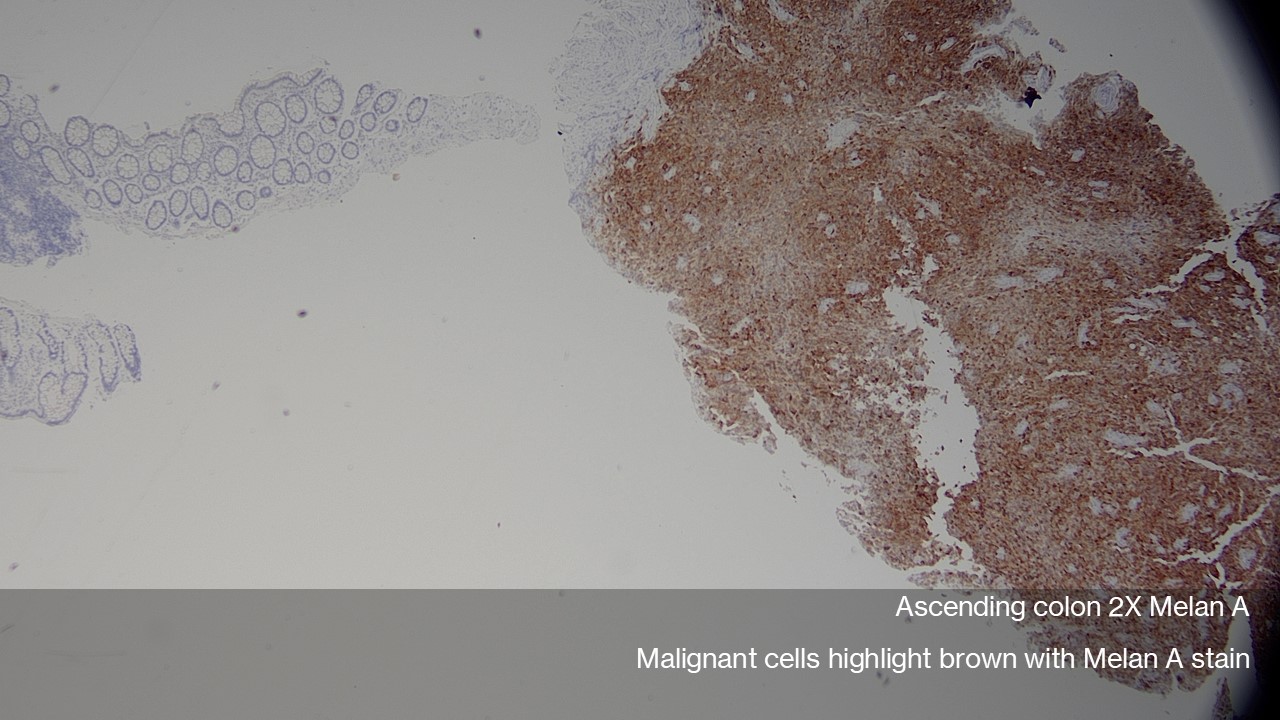
Esophagogastroduodenoscopy (EGD) revealed a benign-appearing 8 mm antral nodule. Colonoscopy showed 13 polyps, including a 15 mm sigmoid lesion. Histopathology demonstrated metastatic melanoma in polyps from the transverse and ascending colon, both arising in a background of tubular adenomas. The remaining polyps were benign tubular or serrated adenomas. Immunohistochemistry confirmed melanocytic origin (SOX-10, MART-1, HMB-45 positive). Immunotherapy was paused due to anemia, and oncology follow-up was arranged.
Discussion:
This case highlights the importance of histological evaluation of colonic polyps in melanoma patients who present with unexplained anemia or GI bleeding. Metastatic melanoma of the colon is extremely uncommon, occurring in 0.3% of patients with primary melanoma. Melanocytic origin is confirmed by immunohistochemical staining, which is frequently associated with markers such as MART-, HMB-45, and SOX-10, as in our case. Management is guided by disease severity, mutation status, and symptom burden, ranging from surgical resection to systemic therapy. First line systemic therapy includes anti–PD–1 agents (e.g. nivolumab, pembrolizumab), alone or with anti–CTLA–4. BRAF V600E/K-mutated tumors may respond to BRAF/MEK inhibitors. In conclusion, awareness of this rare entity is key to accurate diagnosis and timely oncologic management.
Disclosures:
Diksha Kajal, MD1, Rahul Kumar, MD2, Rebecca Radcliffe, DO3, Iryna S. Hepburn, MD, FACG1. P2490 - Beyond the Adenoma: A Rare Case of Colonic Melanoma Metastasis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
