Tuesday Poster Session
Category: Colon
P4655 - Primary Gastrointestinal Plasmablastic Lymphoma in an Immunocompetent Patient Presenting With Chronic Intermittent Diarrhea
- NV
Nicholas P. Valle, MD
University of California Los Angeles David Geffen School of Medicine
Los Angeles, CA
Presenting Author(s)
Nicholas P.. Valle, MD1, Timothy Zaki, MD1, Michelle Guan, MD2, Jeffrey Li, BA3, Bita Naini, MD4, Jonathan Said, MD1, Guy A. Weiss, MD5
1University of California Los Angeles David Geffen School of Medicine, Los Angeles, CA; 2Ucla, Los Angeles, CA; 3David Geffen School of Medicine at UCLA, Los Angeles, CA; 4UCLA Health, Los Angeles, CA; 5University of California Los Angeles Medical Center, Los Angeles, CA
Introduction:
We report a case of an immunocompetent adult male with a two-year history of episodic diarrhea fulfilling Rome IV criteria for functional diarrhea. However, rising fecal calprotectin prompted further evaluation, ultimately revealing primary plasmablastic lymphoma (PBL) of the terminal ileum and ileocecal valve. PBL is a rare, aggressive variant of diffuse large B-cell lymphoma. This case highlights diagnostic challenges and the importance of maintaining suspicion for malignancy in patients with unexplained gastrointestinal (GI) symptoms.
Case Description/Methods:
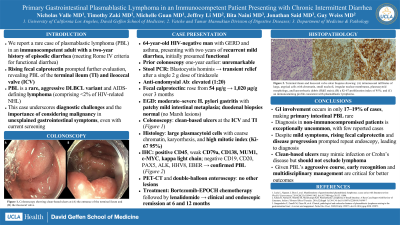
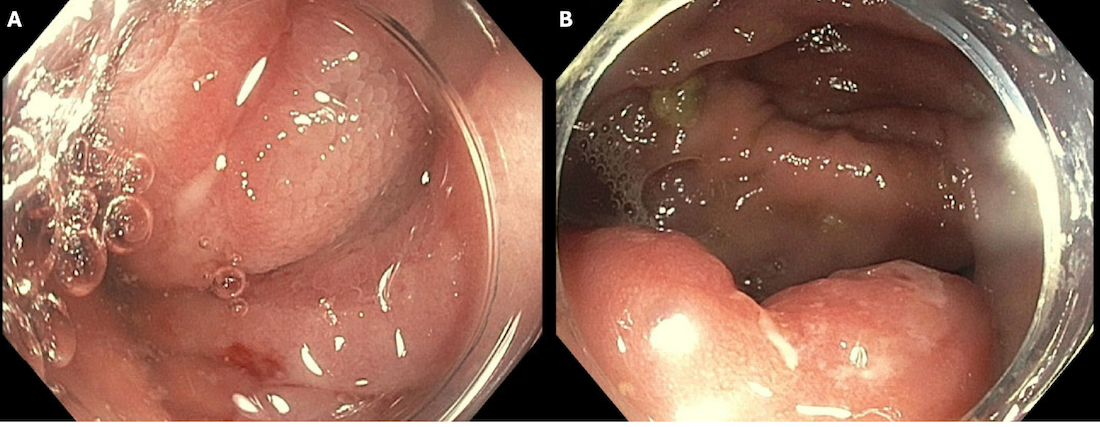
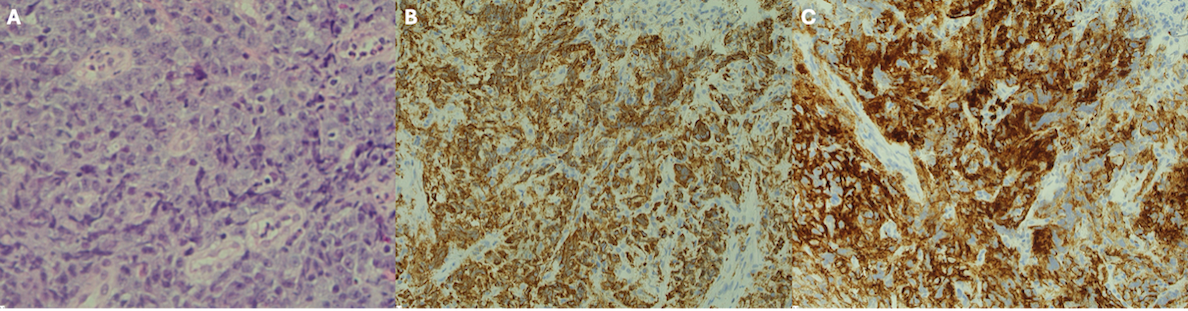
A 64-year-old HIV-negative male with GERD and asthma reported recurrent mild diarrhea over two years, initially presumed functional. Colonoscopy one year prior was unremarkable. Stool PCR detected Blastocystis hominis, with transient relief from metronidazole. Anti-endomysial antibodies were elevated. Fecal calprotectin rose significantly from borderline (54 µg/g) to markedly elevated (1020 µg/g) over three months. Upper endoscopy revealed moderate to severe H. pylori gastritis with patchy mild intestinal metaplasia; duodenal biopsies were normal with no celiac disease. Colonoscopy revealed clean-based ulcers at the ileocecal valve and terminal ileum. (Figure 1). Biopsies showed large, plasmacytoid cells with coarse chromatin, small nucleoli, karyorrhectic debris, and high mitotic index (Ki-67: 95%). Immunostaining was positive for CD45, weak CD79a, CD138, MUM1, c-MYC, and kappa light chain; negative for CD19, CD20, PAX5, ALK, HHV8, and EBV-encoded RNA (Figure 2), confirming PBL. PET-CT and double balloon enteroscopy showed no other lesions. Treatment with Bortezomib-EPOCH chemotherapy followed by lenalidomide induced clinical and endoscopic remission.
Discussion:
PBL is a rare AIDS-defining lymphoma, accounting for < 2% of HIV-related non-Hodgkin lymphomas. Approximately 17–19% of cases involve the GI tract, making primary gut-based PBL an uncommon presentation. Diagnosis is even more unusual in immunocompetent, HIV-negative individuals like our patient, with only scattered reports in the literature. Despite a mild clinical presentation, rising fecal calprotectin and symptom progression prompted repeat endoscopic evaluation, leading to the diagnosis of PBL. Importantly, clean-based ileocecal ulcers should not preclude consideration of lymphoma. Given PBL’s aggressive nature and poor prognosis without early treatment, timely recognition and multidisciplinary collaboration is essential.
Disclosures:
Nicholas P.. Valle, MD1, Timothy Zaki, MD1, Michelle Guan, MD2, Jeffrey Li, BA3, Bita Naini, MD4, Jonathan Said, MD1, Guy A. Weiss, MD5. P4655 - Primary Gastrointestinal Plasmablastic Lymphoma in an Immunocompetent Patient Presenting With Chronic Intermittent Diarrhea, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

