Tuesday Poster Session
Category: Colon
P4680 - A Diagnostic Puzzle: GI Amyloidosis Presenting With Non-Specific Colitis-Like Symptoms


Teskey Garrett, DO
Scripps Mercy Hospital
Yorba Linda, CA
Presenting Author(s)
1Scripps Mercy Hospital, Yorba Linda, CA; 2Georgetown Public Hospital Corporation, Georgetown, Demerara-Mahaica, Guyana; 3Scripps Green Hospital, San Diego, CA; 4Scripps Clinic, San Diego, CA; 5Scripps Clinic Medical Group, La Jolla, CA; 6Scripps Clinic Medical Group, San Diego, CA
Introduction:
Amyloidosis is a condition caused by extracellular deposition of misfolded proteins forming β-pleated sheet fibrils that disrupt tissue structure and function. AL amyloidosis, the most common subtype, can involve the gastrointestinal (GI) tract in a subset of patients. GI involvement manifests with diverse symptoms including diarrhea, malabsorption, constipation, bleeding, and pseudo-obstruction. Diagnosis is challenging due to the patchy, submucosal nature of deposits and low sensitivity of mucosal biopsies.
Case Description/Methods:
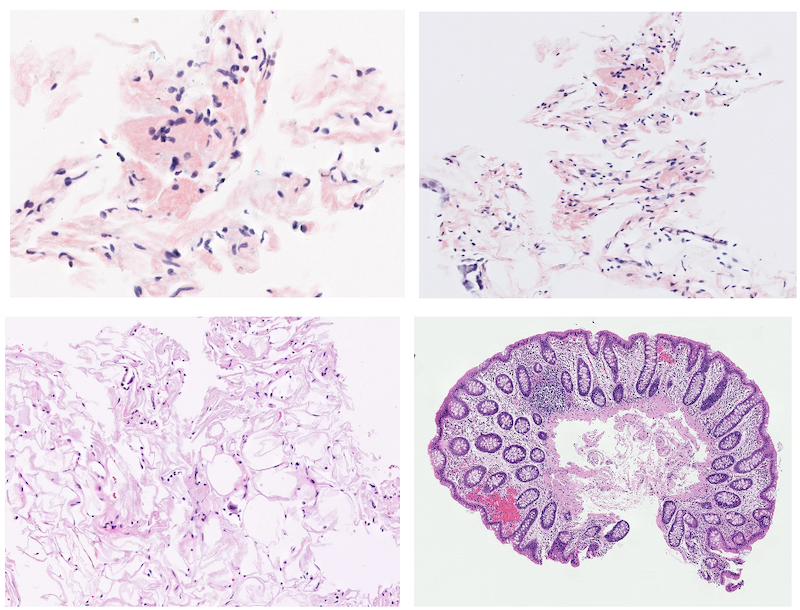
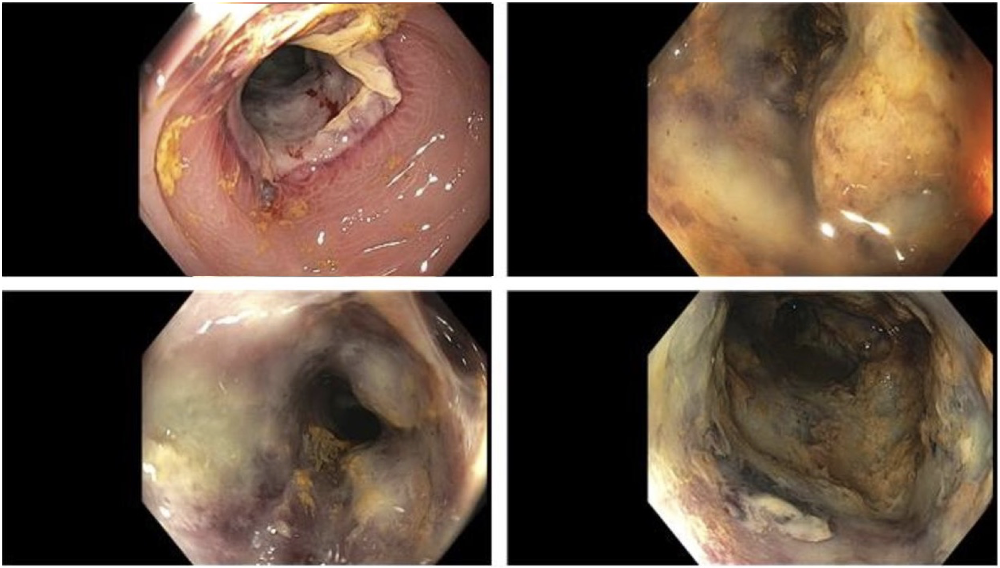
A 72-year-old woman with a history of hypertension, hyperlipidemia, and chronic constipation presented with acute-onset left lower quadrant pain and hematochezia. She reported four to five loose stools per day without precipitating factors. On initial workup her Hgb was 9.7 g/dL, CRP 199 mg/L, calprotectin 790 µg/g, and with mild renal impairment. CT angiography revealed atherosclerosis with patent mesenteric vessels. Colonoscopy showed circumferential sigmoid ulcerations with mucosal edema and histology suggesting chronic active colitis, but negative for Congo red staining.
Subsequent workup revealed proteinuria, an abnormal kappa/lambda ratio (0.06), and bone marrow biopsy with a clonal plasma cell population. Abdominal fat pad biopsy confirmed amyloid deposition. Repeat colonoscopy with extensive biopsies redemonstrated progressive ulceration, luminal narrowing, and biopsy results were positive for Congo red staining with amyloid deposits seen in the vascular wall. Findings supported the diagnosis of systemic AL amyloidosis with GI and renal involvement.
The patient was initiated on daratumumab, cyclophosphamide, bortezomib, and dexamethasone, and follow-up colonoscopy is scheduled after chemotherapy.
Discussion:
GI amyloidosis is notoriously difficult to diagnose due to its patchy submucosal involvement, often sparing mucosal layers accessed during routine biopsy. This patient’s presentation highlights the importance of a high index of suspicion and comprehensive workup. Furthermore, fat pad aspiration remains a valuable, minimally invasive diagnostic tool when mucosal biopsies are inconclusive.
This case emphasizes the diagnostic challenges of GI amyloidosis, particularly when initial investigations are unrevealing. In patients with unexplained GI pathology and systemic findings such as proteinuria or abnormal light chain ratios, clinicians should maintain a high index of suspicion for amyloidosis, even in the absence of histologic confirmation on GI biopsies.
Disclosures:
Garrett Teskey, DO1, Oneka Daniels, MD2, Collin Mayemura, MD3, Emma Du, MD4, Gauree Konijeti, MD, MPH, FACG5, Mazer Ally, MD6. P4680 - A Diagnostic Puzzle: GI Amyloidosis Presenting With Non-Specific Colitis-Like Symptoms, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
