Tuesday Poster Session
Category: Colon
P4691 - One and Done: The Development of a Severe Colonic Stricture After 1 Episode of Bowel Ischemia in a Healthy Middle-Aged Female

Ivana Rubenstein, DO
Broward Health Medical Center
Fort Lauderdale, FL
Presenting Author(s)
1Broward Health Medical Center, Fort Lauderdale, FL; 2Broward Health Medical Center, Miami, FL; 3Gastro Health, Coral Springs, FL
Introduction: Colonic ischemia occurs due to compromised blood flow to the colon, resulting in inflammation and variable injury. Although typically self-limited, severe cases may lead to necrosis, perforation, sepsis, or rarely, colonic stricture formation. These complications usually affect older patients with vascular comorbidities. Stricture formation from a single ischemic event in a healthy individual is rare.
Case Description/Methods:
A 55-year-old previously healthy woman presented with acute lower abdominal pain, nausea, vomiting, and hematochezia after returning from a cruise. CT abdomen/pelvis with IV and oral contrast revealed severe colitis in the transverse and descending colon. Colonoscopy confirmed ischemic colitis; biopsies showed acute colitis with focal acute epithelitis. She was treated with IV piperacillin-tazobactam and discharged after clinical improvement.
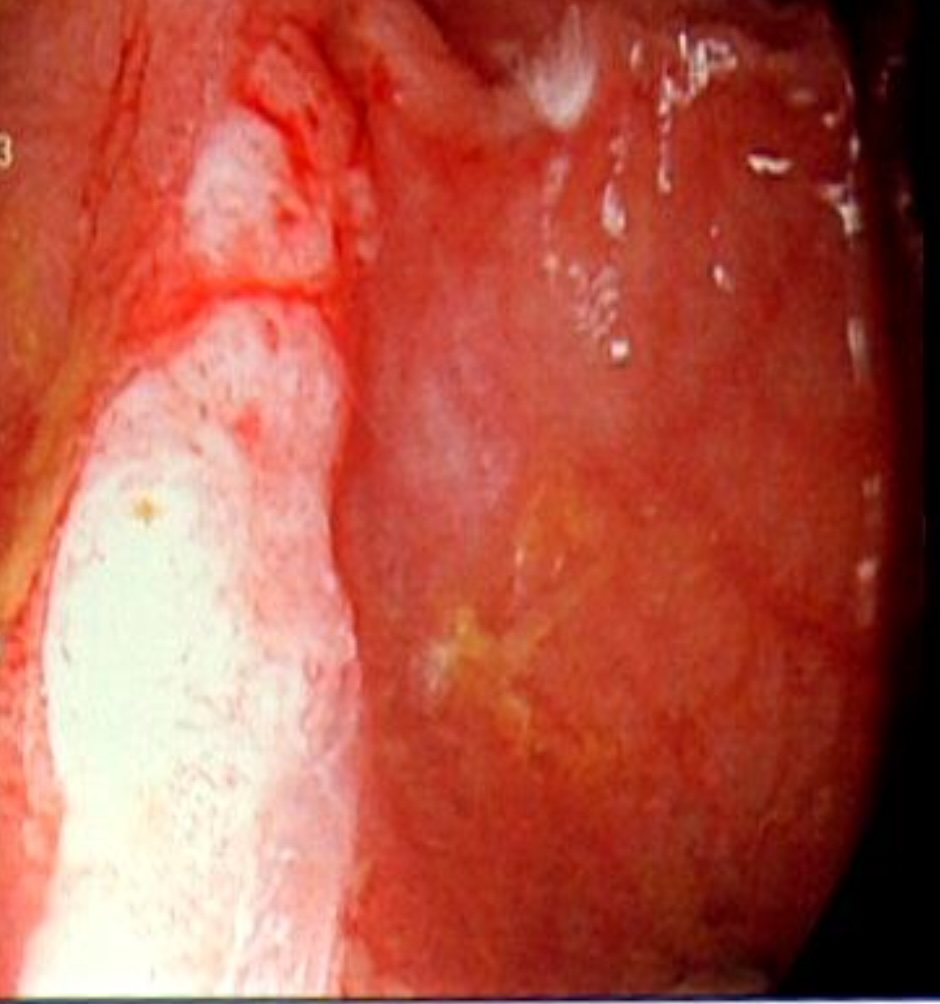
Two weeks later, she developed persistent abdominal pain without bleeding, fever, or constipation. Repeat CT revealed moderate luminal narrowing at the splenic flexure without active inflammation, concerning for a stricture. A follow-up colonoscopy showed a 3–4 cm circumferential ulcerated stricture at the splenic flexure and descending colon. Due to symptom persistence and upstream colonic dilation with fecal impaction, she underwent segmental colectomy with a temporary end-colostomy. Surgical pathology demonstrated mucosal necrosis, atrophy, and vascular congestion consistent with chronic ischemia, with no neoplasia. At three months post-op, she remained symptom-free. Colostomy reversal was successfully performed six months later.
Discussion: Colonic stricture formation post-ischemia is a rare sequela, more often seen in older patients with cardiovascular or metabolic comorbidities. The fibrotic healing response to ischemia can result in lumen narrowing and obstructive symptoms. This case demonstrates that even a single ischemic insult in an otherwise healthy patient can lead to severe outcomes, underscoring the need for clinical vigilance in follow-up care. Clinicians should be aware that colonic strictures may develop following ischemic colitis, even in patients without traditional risk factors. Persistent abdominal symptoms after ischemic injury should prompt timely imaging and endoscopic evaluation to avoid delayed diagnosis and complications.

Disclosures:
Ivana Rubenstein, DO1, Lorraine Chong Tai, MD1, Amanda Eukovich, DO1, Edwin Makarevich, DO1, Andrea Escalante, DO2, Ronen Arai, MD3. P4691 - One and Done: The Development of a Severe Colonic Stricture After 1 Episode of Bowel Ischemia in a Healthy Middle-Aged Female, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
