Tuesday Poster Session
Category: Colon
P4699 - Severe Immunosuppression Revealing High-Grade B-Cell Lymphoma in a Patient With Untreated HIV
.jpg)
Amil Shah, DO
Parkview Medical Center
Pueblo, CO
Presenting Author(s)
Parkview Medical Center, Pueblo, CO
Introduction: HIV infection, if untreated, can lead to significant immunosuppression, ultimately predisposing patients to opportunistic infections and AIDS-defining malignancies such as high-grade B-cell lymphoma. Nonspecific symptoms may be the initial presentation of a serious underlying process. We present a case of newly diagnosed AIDS with gastrointestinal lymphoma, which was initially suspected to be inflammatory bowel disease, as well as opportunistic esophageal candidiasis.
Case Description/Methods:
A 31-year-old male with a history of untreated HIV presented with abdominal pain, unintentional weight loss and occasional night sweats. Initial labs revealed hemoglobin 5.6 g/dL, MCV 84.9 fL, and he received two units of PRBCs. Stool pathogen panel was negative, and fecal calprotectin was not elevated. ESR and CRP were 27 mm/hr and 74 mg/L, respectively. HIV screen showed a positive antibody with a negative p24 antigen. CD4 count was 12 cells/μL, and HIV viral load was 155,000 copies/mL.
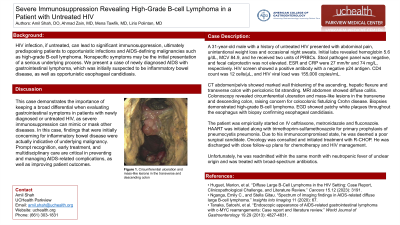
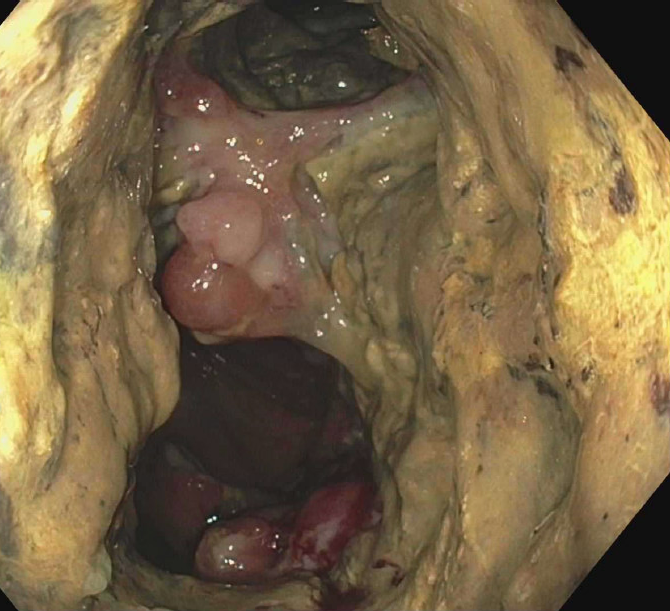
CT abdomen/pelvis showed marked wall thickening of the ascending, hepatic flexure and transverse colon with pericolonic fat stranding. MRI abdomen showed diffuse colitis. Colonoscopy revealed circumferential ulceration and mass-like lesions in the transverse and descending colon, raising concern for colocolonic fistulizing Crohn disease. Biopsies demonstrated high-grade B-cell lymphoma. EGD showed patchy white plaques throughout the esophagus with biopsy confirming esophageal candidiasis.
The patient was empirically started on IV ceftriaxone, metronidazole and fluconazole. HAART was initiated along with trimethoprim-sulfamethoxazole for primary prophylaxis of pneumocystis pneumonia. Due to his immunocompromised state, he was deemed a poor surgical candidate. Oncology was consulted and initiated treatment with R-CHOP. He was discharged with close follow-up plans for chemotherapy and HIV management.
Discussion: This case demonstrates the importance of keeping a broad differential when evaluating gastrointestinal symptoms in patients with newly diagnosed or untreated HIV, as severe immunosuppression can mimic or mask other diseases. In this case, findings that were initially concerning for inflammatory bowel disease were actually indicative of underlying malignancy. Prompt recognition, early treatment, and multidisciplinary care are critical in preventing and managing AIDS-related complications, as well as improving patient outcomes.
Disclosures:
Amil Shah, DO, Ahmad Zain, MBBS, Mena Tawfik, MD, Lirio Polintan, MD. P4699 - Severe Immunosuppression Revealing High-Grade B-Cell Lymphoma in a Patient With Untreated HIV, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
