Tuesday Poster Session
Category: Colon
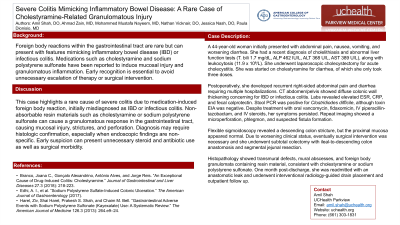
P4700 - Severe Colitis Mimicking Inflammatory Bowel Disease: A Rare Case of Cholestyramine-Related Granulomatous Injury
.jpg)
Amil Shah, DO
Parkview Medical Center
Pueblo, CO
Presenting Author(s)
1Parkview Medical Center, Pueblo, CO; 2UCHealth Parkview Medical Center, Pueblo, CO
Introduction: Foreign body reactions within the gastrointestinal tract are rare but can present with features mimicking inflammatory bowel disease (IBD) or infectious colitis. Medications such as cholestyramine and sodium polystyrene sulfonate have been reported to induce mucosal injury and granulomatous inflammation. Early recognition is essential to avoid unnecessary escalation of therapy or surgical intervention.
Case Description/Methods:
A 44-year-old woman initially presented with abdominal pain, nausea, vomiting, and worsening diarrhea. She had a recent diagnosis of cholelithiasis and abnormal liver function tests (T. bili 1.7 mg/dL, ALP 462 IU/L, ALT 368 U/L, AST 389 U/L), along with leukocytosis (11.9 x 10⁹/L). She underwent laparoscopic cholecystectomy for acute cholecystitis. She was started on cholestyramine for diarrhea, of which she only took three doses.
Postoperatively, she developed recurrent right-sided abdominal pain and diarrhea requiring multiple hospitalizations. CT abdomen/pelvis showed diffuse colonic wall thickening concerning for IBD or infectious colitis. Labs revealed elevated ESR, CRP, and fecal calprotectin. Stool PCR was positive for Clostridiodes difficile, although toxin EIA was negative. Her symptoms persisted despite oral vancomycin, fidaxomicin, IV piperacillin-tazobactam, and IV steroids. Repeat imaging showed a microperforation, phlegmon, and suspected fistula formation.
Flexible sigmoidoscopy revealed a descending colon stricture with normal proximal mucosa. Eventually, she underwent subtotal colectomy with ileal-to-descending colon anastomosis and segmental jejunal resection.
Histopathology showed transmural defects, mural abscesses, and foreign body granulomata containing resin material, consistent with cholestyramine or sodium polystyrene sulfonate. One month after discharge, she was readmitted with an anastomotic leak and underwent interventional radiology-guided drain placement and outpatient follow up.
Discussion: This case highlights a rare cause of severe colitis due to medication-induced foreign body reaction, initially misdiagnosed as IBD or infectious colitis. Non-absorbable resin materials such as cholestyramine or sodium polystyrene sulfonate can cause a granulomatous response in the gastrointestinal tract, causing mucosal injury, strictures, and perforation. Diagnosis may require confirmation by histology, especially when endoscopic findings are non-specific. Early suspicion can present unnecessary steroid and antibiotic use as well as surgical morbidity.
Disclosures:
Amil Shah, DO1, Ahmad Zain, MBBS1, Mustafa Nayeem, MD1, Nathan Vicknair, MD2, Jessica Nash, DO1, Paula Dionisio, MD1. P4700 - Severe Colitis Mimicking Inflammatory Bowel Disease: A Rare Case of Cholestyramine-Related Granulomatous Injury, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
