Tuesday Poster Session
Category: Colon
P4709 - Chicken or the Egg: An Interesting Case of Ogilvie Syndrome in a Schizophrenic Patient with Recent Clozapine Use and Concurrent Acute Herpes Zoster Infection

Jason Truong, DO, MS
HCA Medical City Healthcare UNT-TCU GME (Arlington)
Arlington, TX
Presenting Author(s)
1HCA Medical City Healthcare UNT-TCU GME (Arlington), Arlington, TX; 2American University of the Caribbean School of Medicine, Miami, FL
Introduction:
Ogilvie Syndrome, or acute colonic pseudo-obstruction, is a rare but serious condition characterized by massive colonic dilatation in the absence of a mechanical blockage. It is often associated with autonomic dysregulation and certain medications. Clozapine, an atypical antipsychotic with potent anticholinergic effects, has been implicated in GI hypomotility. We report a unique case of Ogilvie Syndrome in a schizophrenic patient recently started on clozapine, complicated by acute shingles.
Case Description/Methods:
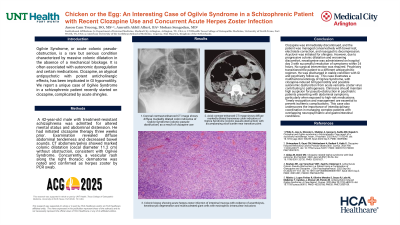
A 42-year-old male with treatment-resistant schizophrenia was admitted for altered mental status and abdominal distension. He had initiated clozapine therapy three weeks prior. Examination revealed diffuse abdominal tenderness and decreased bowel sounds. CT abdomen/pelvis showed marked colonic dilatation (cecal diameter 11.2 cm) without obstruction, consistent with Ogilvie Syndrome. Concurrently, a vesicular rash along the right thoracic dermatome was noted and confirmed as herpes zoster by PCR swab.
Discussion:
Clozapine was immediately discontinued, and the patient was managed conservatively with bowel rest, electrolyte correction, and nasogastric decompression. Acyclovir was initiated for shingles. However, due to progressive colonic dilatation and worsening discomfort, neostigmine was administered on hospital day 3 with successful resolution of symptoms within 24 hours. No surgical intervention was required. Psychiatry transitioned the patient to a different antipsychotic regimen. He was discharged in stable condition with GI and psychiatry follow-up.
This case illustrates a multifactorial etiology of Ogilvie Syndrome, with clozapine-induced GI hypomotility and possible autonomic dysfunction from acute varicella-zoster virus contributing to pathogenesis. Clinicians should maintain high suspicion for pseudo-obstruction in psychiatric patients presenting with abdominal symptoms, particularly when exposed to high-risk medications. Timely recognition and management are essential to prevent ischemic complications. This case also underscores the importance of interdisciplinary coordination in managing complex patients with overlapping neuropsychiatric and gastrointestinal conditions.
Disclosures:
Jason C. Truong, DO, MS1, Amruth A. Alluri, BA2. P4709 - Chicken or the Egg: An Interesting Case of Ogilvie Syndrome in a Schizophrenic Patient with Recent Clozapine Use and Concurrent Acute Herpes Zoster Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
