Tuesday Poster Session
Category: Colon
P4710 - Recurrent Pancreatic Cancer With Metastasis to the Sigmoid Colon: A Case Report
- JH
Joann Ha, DO
Jefferson Health
Voorhees, NJ
Presenting Author(s)
1Jefferson Health, Voorhees, NJ; 2Jefferson Health, Cherry Hill, NJ; 3Jefferson Health, Sewell, NJ
Introduction: Pancreatic ductal adenocarcinoma (PDAC) is an aggressive malignancy with a high propensity for local invasion and distant metastasis, most commonly to the liver, lungs, and peritoneum. Metastasis to the colon, particularly presenting as a clinically significant stricture or mass, is exceedingly rare and represents an unusual manifestation of disease progression.
Case Description/Methods:
A 74-year-old male with a significant past medical history of stage IIIB pancreatic adenocarcinoma, status post distal pancreatectomy and splenectomy with adjuvant chemotherapy and radiation, as well as a history of sigmoid colon cancer, presented with abdominal pain.
He was evaluated by oncology in the outpatient setting after a recent computed tomography (CT) scan demonstrated local progression of his pancreatic cancer. The patient had previously received multiple lines of therapy, including adjuvant capecitabine with gemcitabine, followed by chemoradiation after undergoing a Whipple procedure. A prior PET scan had demonstrated hypermetabolic activity in several locations: the left retroperitoneum (between the adrenal gland and aorta), lower abdominal wall musculature, and sigmoid colon.
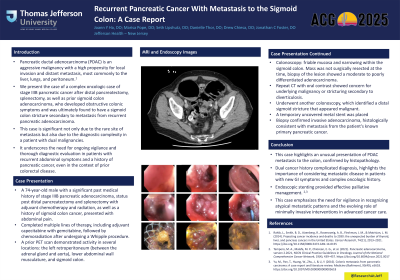
Given these findings, the patient underwent colonoscopy, which revealed friable mucosa and narrowing within the sigmoid colon. Although the mass was not surgically resected at the time, biopsy of the lesion showed a moderate to poorly differentiated adenocarcinoma. A repeat CT with oral contrast again showed persistent sigmoid wall thickening, possibly related to an underlying malignancy or stricturing secondary to diverticulosis. To address the sigmoid obstruction, the patient underwent another colonoscopy, which identified a distal sigmoid stricture that appeared malignant. A temporary uncovered metal stent was placed to relieve the obstruction. Biopsy of the stricture confirmed invasive adenocarcinoma, histologically consistent with metastasis from the patient's known primary pancreatic cancer.
Discussion: This case highlights an unusual presentation of PDAC metastasis to the colon, confirmed by histopathology. The patient’s dual cancer history complicated diagnosis, highlights the importance of considering metastatic disease in patients with new GI symptoms and complex oncologic history. Endoscopic stenting provided effective palliative management. This case emphasizes the need for vigilance in recognizing atypical metastatic patterns and the evolving role of minimally invasive interventions in advanced cancer care.
Disclosures:
Joann Ha, DO1, Marisa Pope, DO2, Seth Lipshutz, DO2, Danielle Thor, DO, MAUB3, Drew Chiesa, DO3, C. Jonathan Foster, DO3. P4710 - Recurrent Pancreatic Cancer With Metastasis to the Sigmoid Colon: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
