Tuesday Poster Session
Category: Colon
P4714 - When Youth Is Misleading: Critical Management of Intussusception in a Young Adult

Ahmed Shehadah, MD
United Health Services, Wilson Medical Center
Binghamton, NY
Presenting Author(s)
1United Health Services, Wilson Medical Center, Binghamton, NY; 2Rochester General Hospital, Rochester, NY; 3SUNY Upstate Medical University, Syracuse, NY; 4United Health Services, Wilson Medical Center, Johnson City, NY; 5United Health Services, Johnson City, NY
Introduction: Intussusception is managed differently in children and adults, with pediatric cases often treated conservatively and adult cases typically requiring surgical intervention due to the higher likelihood of malignancy. Management becomes less clear when intussusception presents in early adulthood. We present a rare case of intussusception in a young adult, highlighting the diagnostic process, management approach, and the importance of early intervention.
Case Description/Methods:
A 27-year-old male with no significant past medical history presented to the emergency room with abdominal pain, nausea, and hematochezia. Vital signs were stable, and laboratory workup, including tumor markers, was unremarkable. Contrast-enhanced computed tomography of the abdomen and pelvis showed a mid-transverse colon intussusception but did not show any mass.
A small bowel follow-through confirmed a partially obstructing intussusception in the transverse colon, and a normal proximal colon. The differential diagnosis included a pathological lead point due to submucosal lymphoid hyperplasia, lipoma, infectious or inflammatory etiologies, malignancy and others.
Colonoscopy was performed to rule out malignancy, and revealed a 46 mm polypoid lesion in the proximal transverse colon, and the area was tattooed for localization. The patient subsequently underwent laparoscopic right colectomy.
Histopathology demonstrated invasive, poorly differentiated mucinous adenocarcinoma of the colon, with invasion into the muscularis propria and subserosal fibroadipose tissue. Resection margins were uninvolved, and all 58 resected lymph nodes were negative. The tumor was classified as stage II mucinous adenocarcinoma. Given the absence of BRAF mutation and MLH1 promoter hypermethylation, genetic germline testing was recommended to evaluate for Lynch syndrome.
Discussion: This case highlights the importance of maintaining a high index of suspicion in cases of intussusception. Unlike pediatric intussusception, which is typically idiopathic and managed conservatively, adult intussusception often indicates an underlying malignancy and warrants early surgical evaluation. In this young adult, prompt endoscopic and surgical intervention led to the early diagnosis and treatment prior to metastatic spread. This case reinforces that young adult patients should be managed according to adult protocols and low threshold for endoscopic evaluation if lesion is within reach.

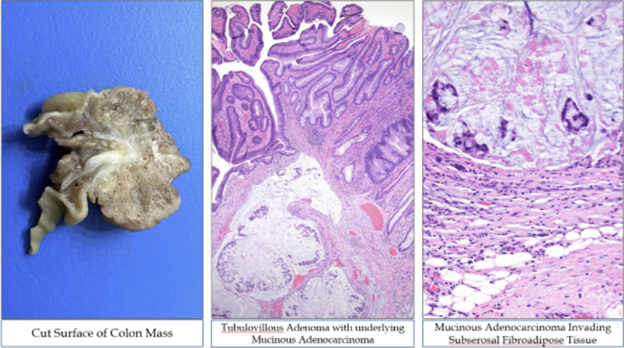
Middle image: Tubulovillous adenoma with underlying mucinous adenocarcinoma
Right Image: Mucinous adenocarcinoma invading subserosal fibroadipose tissue
Disclosures:
Ahmed Shehadah, MD1, Alshaima Yousef, MD2, Timothy Chan, BS3, Usama Sakhawat, MD4, Khandokar Talib, MD5, Joseph Jones, MD4, Minhaz Ahmad, MD1, Toseef Javaid, MD4, Amanke Oranu, MD1. P4714 - When Youth Is Misleading: Critical Management of Intussusception in a Young Adult, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
