Tuesday Poster Session
Category: Esophagus
P4982 - POSTER WITHDRAWN
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Has Audio
Rhett Harmon, MD1, Nicholas Cheung, MD2, Dorian Mendoza, MD3, Shaun Chandna, DO2, Daniel Cole, MD, MPH1
1Olive View-UCLA Medical Center, Los Angeles, CA; 2Olive View-UCLA Medical Center, Sylmar, CA; 3David Geffen School of Medicine at UCLA, Los Angeles, CA
Introduction: Foreign body ingestion is a common phenomenon, especially in pediatric or elderly populations, and can have risk of severe morbidity and mortality. Complications may range from temporary dysphagia to ulceration with odynophagia, complete obstruction with pulmonary aspiration, or even formation of fistulae. We report a unique case of foreign body ingestion with esophago-pericardial fistulization and cardiac tamponade requiring Video-Assisted Thoracic Surgery (VATS) pericardial window creation.
Case Description/Methods: A 42-year-old male with diabetes and no surgical history presented to the emergency department for chest and back pain occurring after eating breakfast several days prior. He was tachycardic, tachypneic, and hypotensive with jugular venous distention and distant heart sounds on exam. Chest X-ray was significant for widened mediastinum. Bedside echocardiogram revealed large pericardial effusion with evidence of cardiac tamponade. Emergent pericardiocentesis was performed with removal of 450 mL purulent fluid. Gram stain of the pericardial fluid showed Streptococcus constellatus, an oral bacterium, indicative of esophageal-pericardial communication. Foreign body in the distal esophagus was detected on CT chest. EGD revealed concern for extraluminal migration of the foreign body. Due to persistent purulent drainage and clinical deterioration, the patient was transferred for VATS pericardial window placement. He gradually improved without fluid re-accumulation and the pericardial drain was eventually removed without complication. He was treated with ceftriaxone 2 gm daily inpatient and discharged with amoxicillin/clavulanic acid for 6 week total course.
Discussion: This case of esophago-pericardial fistula with pericardial effusion leading to hemodynamic instability and cardiac tamponade highlights the importance of considering esophageal perforation in the differential diagnosis of patients presenting with chest pain following meals and whom have signs of infection, particularly if history is concerning for foreign body ingestion. The presence of Streptococcus constellatus, an oral bacterium, in the pericardial fluid was a key diagnostic finding, highly suggestive of a communication between the esophagus and pericardium. Esophageal perforation is a rare but potentially fatal complication of foreign body ingestion with overall mortality rates approaching 20%. Prompt recognition and treatment of this rare complication is essential in effort to improve outcomes.

Disclosures:
Rhett Harmon, MD1, Nicholas Cheung, MD2, Dorian Mendoza, MD3, Shaun Chandna, DO2, Daniel Cole, MD, MPH1. P4982 - POSTER WITHDRAWN, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Olive View-UCLA Medical Center, Los Angeles, CA; 2Olive View-UCLA Medical Center, Sylmar, CA; 3David Geffen School of Medicine at UCLA, Los Angeles, CA
Introduction: Foreign body ingestion is a common phenomenon, especially in pediatric or elderly populations, and can have risk of severe morbidity and mortality. Complications may range from temporary dysphagia to ulceration with odynophagia, complete obstruction with pulmonary aspiration, or even formation of fistulae. We report a unique case of foreign body ingestion with esophago-pericardial fistulization and cardiac tamponade requiring Video-Assisted Thoracic Surgery (VATS) pericardial window creation.
Case Description/Methods: A 42-year-old male with diabetes and no surgical history presented to the emergency department for chest and back pain occurring after eating breakfast several days prior. He was tachycardic, tachypneic, and hypotensive with jugular venous distention and distant heart sounds on exam. Chest X-ray was significant for widened mediastinum. Bedside echocardiogram revealed large pericardial effusion with evidence of cardiac tamponade. Emergent pericardiocentesis was performed with removal of 450 mL purulent fluid. Gram stain of the pericardial fluid showed Streptococcus constellatus, an oral bacterium, indicative of esophageal-pericardial communication. Foreign body in the distal esophagus was detected on CT chest. EGD revealed concern for extraluminal migration of the foreign body. Due to persistent purulent drainage and clinical deterioration, the patient was transferred for VATS pericardial window placement. He gradually improved without fluid re-accumulation and the pericardial drain was eventually removed without complication. He was treated with ceftriaxone 2 gm daily inpatient and discharged with amoxicillin/clavulanic acid for 6 week total course.
Discussion: This case of esophago-pericardial fistula with pericardial effusion leading to hemodynamic instability and cardiac tamponade highlights the importance of considering esophageal perforation in the differential diagnosis of patients presenting with chest pain following meals and whom have signs of infection, particularly if history is concerning for foreign body ingestion. The presence of Streptococcus constellatus, an oral bacterium, in the pericardial fluid was a key diagnostic finding, highly suggestive of a communication between the esophagus and pericardium. Esophageal perforation is a rare but potentially fatal complication of foreign body ingestion with overall mortality rates approaching 20%. Prompt recognition and treatment of this rare complication is essential in effort to improve outcomes.
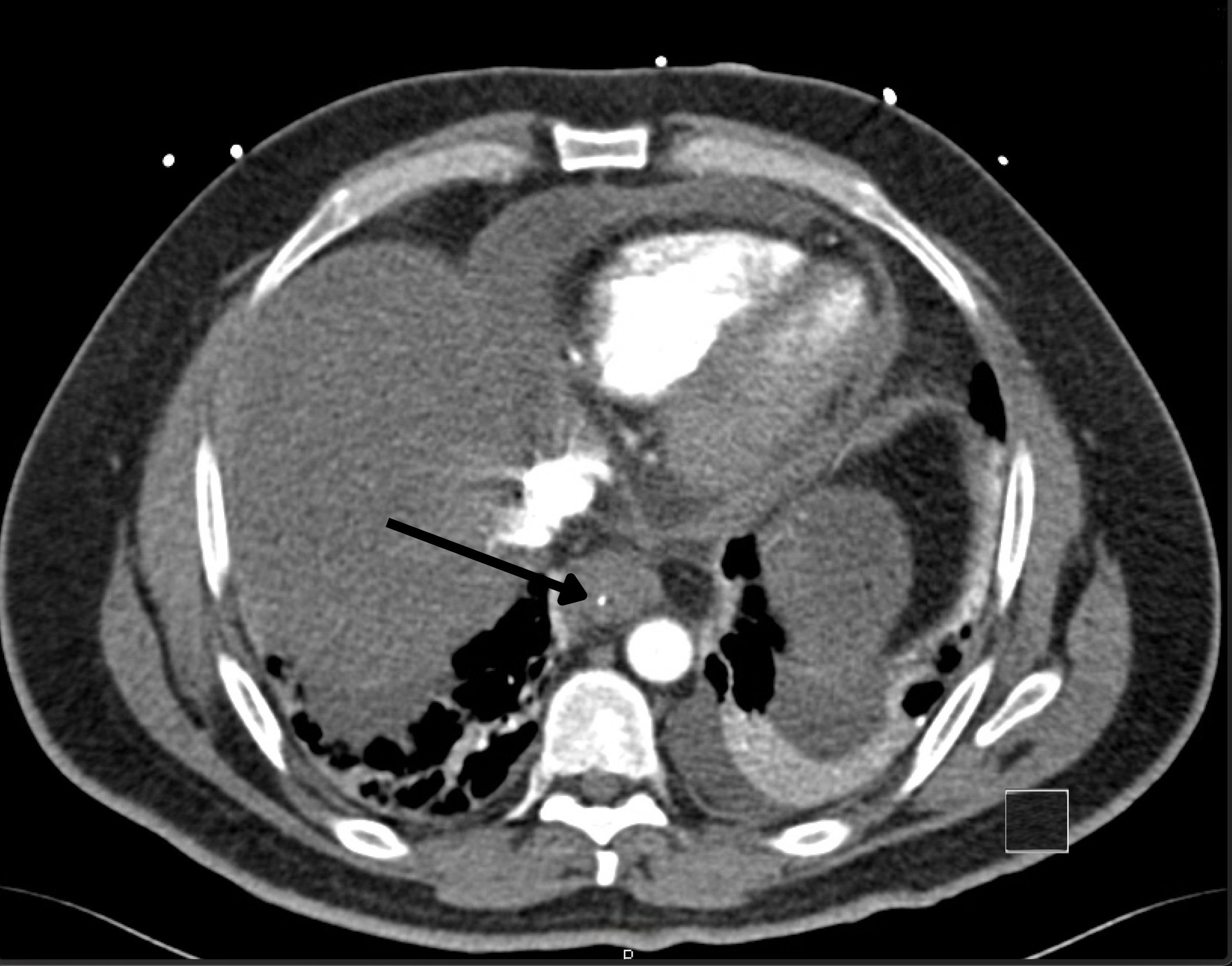
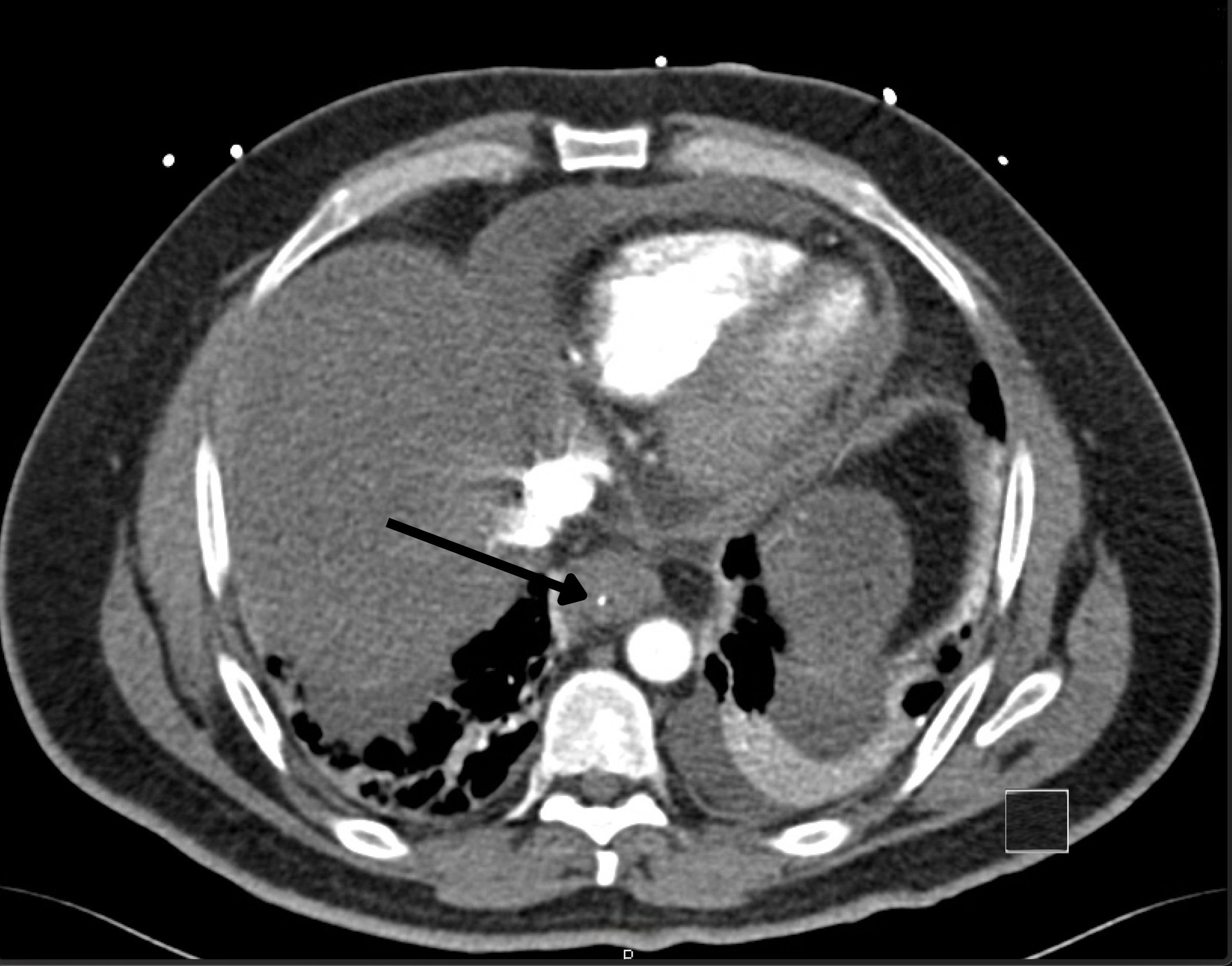
Figure: Distal esophageal mural thickening/esophagitis with indwelling linear radiodensity within the distal esophagus.

Figure: Buried object in distal esophagus: Thin, linear, possibly plastic object penetrating through wall of esophagus.
Disclosures:
Rhett Harmon indicated no relevant financial relationships.
Nicholas Cheung indicated no relevant financial relationships.
Dorian Mendoza indicated no relevant financial relationships.
Shaun Chandna: Arrowhead Pharmaceuticals – Grant/Research Support. Calliditas Therapeutics (formerly Genkyotex) – Grant/Research Support. Ipsen – Consultant. Lipocine – Grant/Research Support. Mirum Pharmaceuticals – Consultant, Grant/Research Support.
Daniel Cole indicated no relevant financial relationships.
Rhett Harmon, MD1, Nicholas Cheung, MD2, Dorian Mendoza, MD3, Shaun Chandna, DO2, Daniel Cole, MD, MPH1. P4982 - POSTER WITHDRAWN, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
