Tuesday Poster Session
Category: Infections and Microbiome
P5565 - Comparison of the Efficacy and Safety of Live Fecal Microbiota Therapeutics for Recurrent Clostridioides difficile Infection (CDI): Matching-Adjusted Indirect Treatment Comparison in Patients With ≥1 CDI Recurrence
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Has Audio
- DN
Dianne Nguyen, MD
Nestlé Health Science
Bridgewater, NJ
Presenting Author(s)
Conor McCloskey, PhD, BSc1, Corinne Le Reun, 1, Dianne Nguyen, MD2, Carl V. Crawford, MD3, Darrell Pardi, MD, MS, FACG4, Morteza Yazdani, PhD5, Mark Wilcox, MD6
1Clarivate Analytics Ltd, London, England, United Kingdom; 2Nestlé Health Science, Bridgewater, NJ; 3NewYork-Presbyterian / Weill Cornell Medical Center, New York, NY; 4Mayo Clinic, Rochester, MN; 5Nestle Health Science, Vevey, Vaud, Switzerland; 6Microbiology & Leeds Institute of Medical Research, Leeds Teaching Hospitals & University of Leeds, Leeds, England, United Kingdom
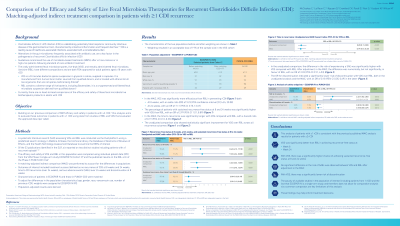
Introduction: Alterations in the gut microbiome, frequently associated with antibiotic use, are a key factor in the pathogenesis of recurrent Clostridioides difficile infection (rCDI). Guidelines recommend microbiota-based treatments (MBTs) after ≥2 recurrences or in high-risk patients. The orally administered fecal microbiota spores, live-brpk (VOS) and rectally administered fecal microbiota, live-jslm (RBL), with different compositions, are both FDA-approved for any patients with rCDI. We previously reported a comparison of the efficacy and safety of these MBTs for the prevention of rCDI using data from randomized controlled trials (RCTs) in patients with ≥2 rCDI.1 This analysis focusses on patients with ≥1 rCDI.
Methods: A systematic literature search (SLR) assessing VOS and RBL was conducted via the Ovid platform using a predefined search strategy in Medline, Embase, the Cochrane library, the Database of Abstracts of Reviews of Effects, and the Health Technology Assessment Database to examine the MBTs of interest. The efficacy and safety of VOS and RBL in this population were compared using individual patient data (IPD) from the VOS single arm study ECOSPOR IV and the published results on the RBL arm of the PUNCH-CD3 study via a matching-adjusted indirect comparison (MAIC) to account for the differences in populations. Outcomes of interest included treatment success (defined as no recurrence of CDI) at 8 weeks, time to CDI recurrence (over 24 weeks) and serious adverse events (SAE) over 24 weeks.
Results: Of the 33 publications identified in the SLR, six, reporting on two distinct studies including patients with ≥1 recurrent episode were deemed eligible for the MAIC. VOS was significantly more efficacious than RBL in preventing rCDI at 8 weeks (odds ratio [OR]; 9.23 [95% confidence interval (CI): 4.24, 20.08]). The time to recurrence over time was significantly lower with VOS compared with RBL (hazard ratio; 0.19 [95% CI; 0.10, 0.33]). There was no significant difference in the risk of having an SAE over 24 weeks with VOS compared with RBL (OR; 2.03 [95% Cl; 0.91, 4.53]).
Discussion: The IPD (≥1 rCDI) analysis is consistent with the previously published MAIC analysis results (≥2 rCDI), significantly favoring VOS over RBL for the clinical outcomes evaluated, with a similar SAE profile.
Disclosures:
Conor McCloskey, PhD, BSc1, Corinne Le Reun, 1, Dianne Nguyen, MD2, Carl V. Crawford, MD3, Darrell Pardi, MD, MS, FACG4, Morteza Yazdani, PhD5, Mark Wilcox, MD6. P5565 - Comparison of the Efficacy and Safety of Live Fecal Microbiota Therapeutics for Recurrent <i>Clostridioides difficile</i> Infection (CDI): Matching-Adjusted Indirect Treatment Comparison in Patients With ≥1 CDI Recurrence, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Clarivate Analytics Ltd, London, England, United Kingdom; 2Nestlé Health Science, Bridgewater, NJ; 3NewYork-Presbyterian / Weill Cornell Medical Center, New York, NY; 4Mayo Clinic, Rochester, MN; 5Nestle Health Science, Vevey, Vaud, Switzerland; 6Microbiology & Leeds Institute of Medical Research, Leeds Teaching Hospitals & University of Leeds, Leeds, England, United Kingdom
Introduction: Alterations in the gut microbiome, frequently associated with antibiotic use, are a key factor in the pathogenesis of recurrent Clostridioides difficile infection (rCDI). Guidelines recommend microbiota-based treatments (MBTs) after ≥2 recurrences or in high-risk patients. The orally administered fecal microbiota spores, live-brpk (VOS) and rectally administered fecal microbiota, live-jslm (RBL), with different compositions, are both FDA-approved for any patients with rCDI. We previously reported a comparison of the efficacy and safety of these MBTs for the prevention of rCDI using data from randomized controlled trials (RCTs) in patients with ≥2 rCDI.1 This analysis focusses on patients with ≥1 rCDI.
Methods: A systematic literature search (SLR) assessing VOS and RBL was conducted via the Ovid platform using a predefined search strategy in Medline, Embase, the Cochrane library, the Database of Abstracts of Reviews of Effects, and the Health Technology Assessment Database to examine the MBTs of interest. The efficacy and safety of VOS and RBL in this population were compared using individual patient data (IPD) from the VOS single arm study ECOSPOR IV and the published results on the RBL arm of the PUNCH-CD3 study via a matching-adjusted indirect comparison (MAIC) to account for the differences in populations. Outcomes of interest included treatment success (defined as no recurrence of CDI) at 8 weeks, time to CDI recurrence (over 24 weeks) and serious adverse events (SAE) over 24 weeks.
Results: Of the 33 publications identified in the SLR, six, reporting on two distinct studies including patients with ≥1 recurrent episode were deemed eligible for the MAIC. VOS was significantly more efficacious than RBL in preventing rCDI at 8 weeks (odds ratio [OR]; 9.23 [95% confidence interval (CI): 4.24, 20.08]). The time to recurrence over time was significantly lower with VOS compared with RBL (hazard ratio; 0.19 [95% CI; 0.10, 0.33]). There was no significant difference in the risk of having an SAE over 24 weeks with VOS compared with RBL (OR; 2.03 [95% Cl; 0.91, 4.53]).
Discussion: The IPD (≥1 rCDI) analysis is consistent with the previously published MAIC analysis results (≥2 rCDI), significantly favoring VOS over RBL for the clinical outcomes evaluated, with a similar SAE profile.
Disclosures:
Conor McCloskey: Clarivate Analytics Ltd – Employee.
Corinne Le Reun: Clarivate Analytics Ltd – Employee.
Dianne Nguyen: Nestlé Health Science – Employee.
Carl Crawford: Ferring – Advisor or Review Panel Member, Consultant, Grant/Research Support, Speakers Bureau. lumen – Grant/Research Support. nestle – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Phathom – Speakers Bureau. vedanta – Grant/Research Support.
Darrell Pardi: Applied Molecular Transport – Consultant. ExeGI Pharma LC – Grant/Research Support. Janssen – Advisory Committee/Board Member. Lilly Medical – Consultant. Pfizer – Consultant. Rise Therapeutics – Grant/Research Support. Takeda – Consultant. Vedanta Bio Sciences INC – Grant/Research Support.
Morteza Yazdani: Nestlé Health Science – Employee.
Mark Wilcox: Seres – Advisor or Review Panel Member, Consultant, Grant/Research Support. Tillotts – Advisor or Review Panel Member, Consultant.
Conor McCloskey, PhD, BSc1, Corinne Le Reun, 1, Dianne Nguyen, MD2, Carl V. Crawford, MD3, Darrell Pardi, MD, MS, FACG4, Morteza Yazdani, PhD5, Mark Wilcox, MD6. P5565 - Comparison of the Efficacy and Safety of Live Fecal Microbiota Therapeutics for Recurrent <i>Clostridioides difficile</i> Infection (CDI): Matching-Adjusted Indirect Treatment Comparison in Patients With ≥1 CDI Recurrence, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
