Tuesday Poster Session
Category: Infections and Microbiome
P5570 - Evolving Landscape of Clostridioides difficile-Associated Mortality in the United States: A 21-Year Analysis of National Data
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mythili Menon Pathiyil, MD
Saint Vincent Hospital
Worcester, MA
Presenting Author(s)
Mythili Menon Pathiyil, MD1, Arvind Kumar Venkataramana Raju, MD1, Rutwik Pradeep. Sharma, MD2, Parth Patel, MD3, Asad Ali, MD4
1Saint Vincent Hospital, Worcester, MA; 2University of Michigan-Sparrow Hospital, Lansing, MI; 3Ascension Saint Joseph Hospital, Chicago, IL; 4SUNY Upstate Medical University Hospital, Syracuse, NY
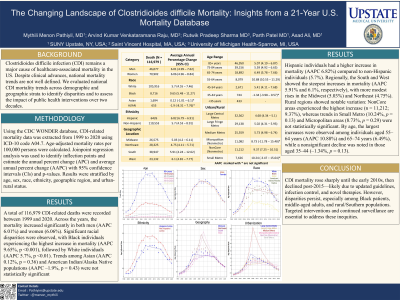
Introduction: Clostridioides difficile infection (CDI) remains a major cause of healthcare-associated mortality in the US despite which national mortality trends remain poorly defined. We assessed CDI mortality trends across demographic and geographic strata to identify disparities and to assess the impact of public health interventions over two decades
Methods: Using CDC WONDER, CDI-related mortality data was extracted from 1999-2020 using ICD-10 code A04.7. Age-adjusted mortality rates per 100,000 persons were calculated. Joinpoint regression was used to identify inflection points and estimate annual percent change(APC) and average annual percent change(AAPC) with 95% confidence intervals(CIs) and p-values. Results were stratified by age, sex, race, ethnicity, geographic region, and urban-rural status
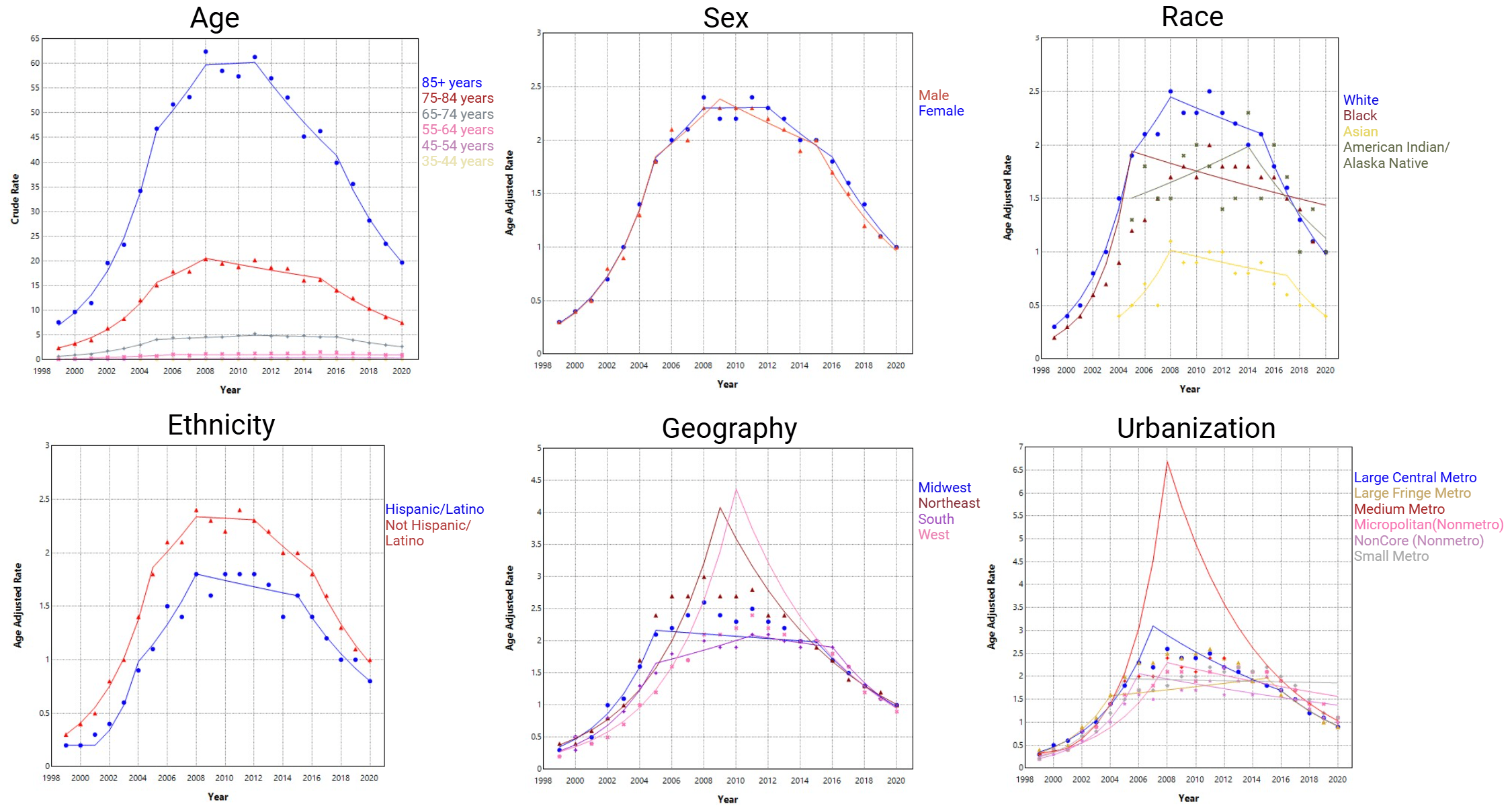
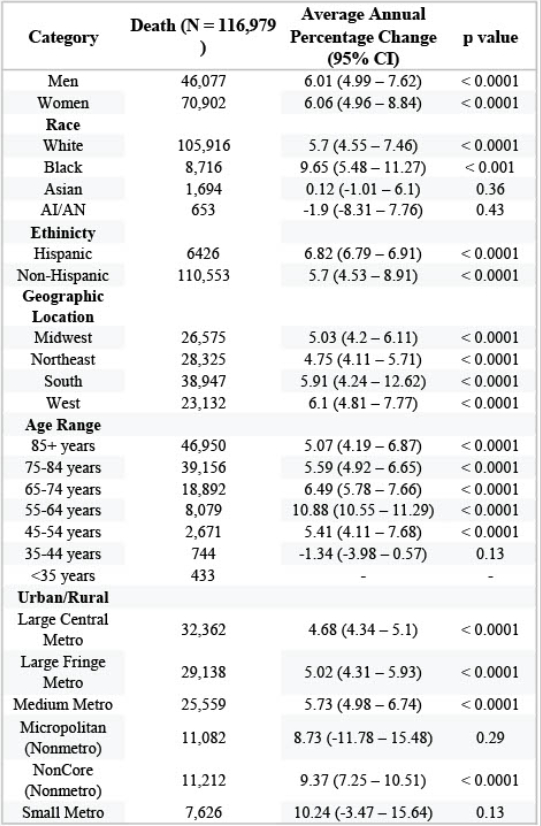
Results: A total of 116,979 CDI-related deaths were recorded between 1999-2020. Across the years the mortality increased significantly in both men (n=46,077; AAPC 6.01%, 95% CI: 4.99–7.62) and women (n=70,902; 6.06%, 95% CI: 4.96–8.84). Significant racial disparities were observed, with Black individuals experiencing the highest increase in mortality (n=8,716; AAPC 9.65%, p=0.0004), followed by White individuals (n=105,916; AAPC 5.7%, p< 0.01). Trends among Asian (AAPC 0.12%, p=0.36) and American Indian/Alaska Native populations (AAPC 1.9%, p=0.43) were not statistically significant. Hispanic individuals (n=6,426) had a higher increase in mortality (AAPC 6.82%) compared to Non-Hispanic individuals (n=110,553; 5.7%). Regionally, the South (n=38,947) and West (n=23,132) showed the steepest increases in mortality (AAPC 5.91% and 6.1%, respectively), with more modest rises in the Midwest (5.03%) and Northeast (4.75%). Rural regions showed notable variation: NonCore areas had the highest increase (n=11,212; 9.37%), though trends in Small Metro (10.24%, p=0.13) and Micropolitan areas (8.73%, p=0.29) were not statistically significant. By age, the largest increases occurred in those aged 55–64 years (n=8,079; AAPC 10.88%) and 65–74 years (n=18,892; 6.49%), while a nonsignificant decline was noted in those aged 35–44 (–1.34%, p=0.13)
Discussion: CDI mortality rose sharply until the early 2010s, then declined post-2015,likely due to updated guidelines, infection control, and novel therapies. However, disparities persist, especially among Black patients, middle-aged adults, and rural/Southern populations. Targeted interventions and continued surveillance are essential to address these inequities
Disclosures:
Mythili Menon Pathiyil, MD1, Arvind Kumar Venkataramana Raju, MD1, Rutwik Pradeep. Sharma, MD2, Parth Patel, MD3, Asad Ali, MD4. P5570 - Evolving Landscape of <i>Clostridioides difficile</i>-Associated Mortality in the United States: A 21-Year Analysis of National Data, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Saint Vincent Hospital, Worcester, MA; 2University of Michigan-Sparrow Hospital, Lansing, MI; 3Ascension Saint Joseph Hospital, Chicago, IL; 4SUNY Upstate Medical University Hospital, Syracuse, NY
Introduction: Clostridioides difficile infection (CDI) remains a major cause of healthcare-associated mortality in the US despite which national mortality trends remain poorly defined. We assessed CDI mortality trends across demographic and geographic strata to identify disparities and to assess the impact of public health interventions over two decades
Methods: Using CDC WONDER, CDI-related mortality data was extracted from 1999-2020 using ICD-10 code A04.7. Age-adjusted mortality rates per 100,000 persons were calculated. Joinpoint regression was used to identify inflection points and estimate annual percent change(APC) and average annual percent change(AAPC) with 95% confidence intervals(CIs) and p-values. Results were stratified by age, sex, race, ethnicity, geographic region, and urban-rural status
Results: A total of 116,979 CDI-related deaths were recorded between 1999-2020. Across the years the mortality increased significantly in both men (n=46,077; AAPC 6.01%, 95% CI: 4.99–7.62) and women (n=70,902; 6.06%, 95% CI: 4.96–8.84). Significant racial disparities were observed, with Black individuals experiencing the highest increase in mortality (n=8,716; AAPC 9.65%, p=0.0004), followed by White individuals (n=105,916; AAPC 5.7%, p< 0.01). Trends among Asian (AAPC 0.12%, p=0.36) and American Indian/Alaska Native populations (AAPC 1.9%, p=0.43) were not statistically significant. Hispanic individuals (n=6,426) had a higher increase in mortality (AAPC 6.82%) compared to Non-Hispanic individuals (n=110,553; 5.7%). Regionally, the South (n=38,947) and West (n=23,132) showed the steepest increases in mortality (AAPC 5.91% and 6.1%, respectively), with more modest rises in the Midwest (5.03%) and Northeast (4.75%). Rural regions showed notable variation: NonCore areas had the highest increase (n=11,212; 9.37%), though trends in Small Metro (10.24%, p=0.13) and Micropolitan areas (8.73%, p=0.29) were not statistically significant. By age, the largest increases occurred in those aged 55–64 years (n=8,079; AAPC 10.88%) and 65–74 years (n=18,892; 6.49%), while a nonsignificant decline was noted in those aged 35–44 (–1.34%, p=0.13)
Discussion: CDI mortality rose sharply until the early 2010s, then declined post-2015,likely due to updated guidelines, infection control, and novel therapies. However, disparities persist, especially among Black patients, middle-aged adults, and rural/Southern populations. Targeted interventions and continued surveillance are essential to address these inequities
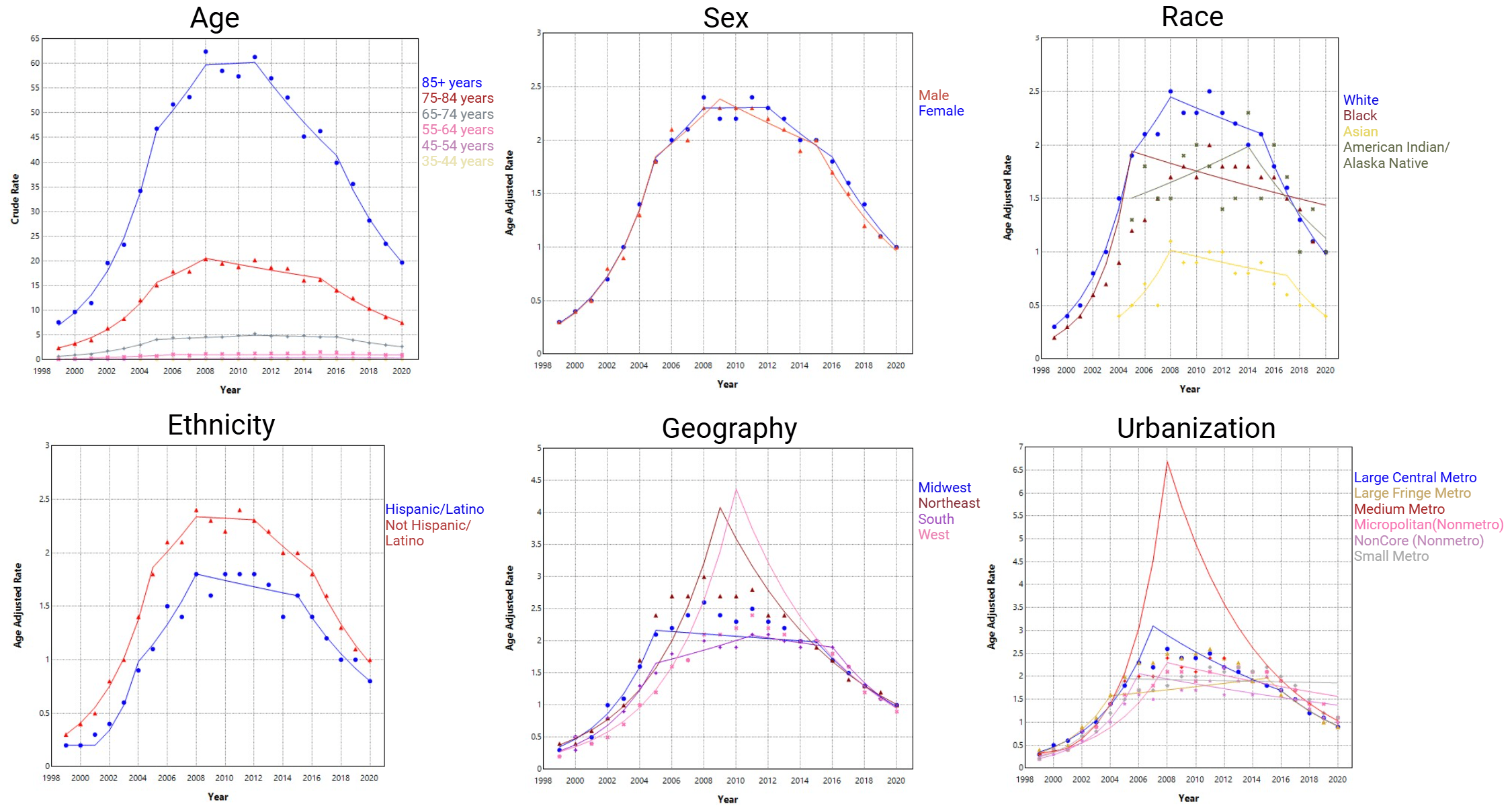
Figure: Table 1: CDI-related deaths, average annual percent change (AAPC), and statistical significance by demographic and geographic subgroup, United States 1999–2020.
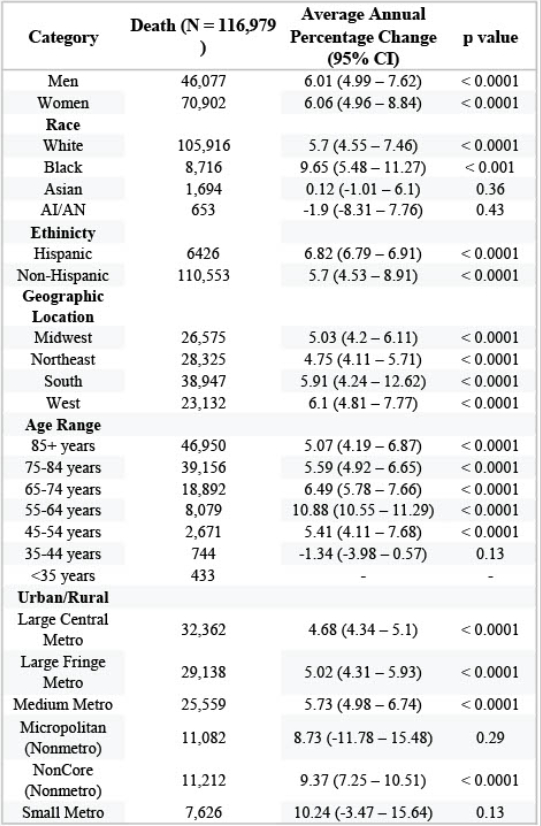
Figure: Figure 1: Joinpoint regression trends in CDI mortality by age, sex, race, ethnicity, region, and urbanicity (1999–2020).
Disclosures:
Mythili Menon Pathiyil indicated no relevant financial relationships.
Arvind Kumar Venkataramana Raju indicated no relevant financial relationships.
Rutwik Sharma indicated no relevant financial relationships.
Parth Patel indicated no relevant financial relationships.
Asad Ali indicated no relevant financial relationships.
Mythili Menon Pathiyil, MD1, Arvind Kumar Venkataramana Raju, MD1, Rutwik Pradeep. Sharma, MD2, Parth Patel, MD3, Asad Ali, MD4. P5570 - Evolving Landscape of <i>Clostridioides difficile</i>-Associated Mortality in the United States: A 21-Year Analysis of National Data, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
