Tuesday Poster Session
Category: Colon
P4723 - Encased Fecalith Masquerading as a Cecal Gastrointestinal Stromal Tumor
- SB
Spencer Birney, BS
The Warren Alpert Medical School of Brown University
Providence, RI
Presenting Author(s)
1The Warren Alpert Medical School of Brown University, Providence, RI; 2Brown University Health, Providence, RI; 3Brown Medicine/Brown Physicians, Inc., Providence, RI
Introduction:
Fecaliths are masses of hardened feces that can mimic neoplastic tumors in appearance. Cecal fecaliths are typically associated with appendicitis. Rare cases have presented as tumor-like lesions unrelated to the appendix. Fecaliths infrequently present as submucosal lesions, and accurate preoperative diagnosis remains challenging. The pathogenesis is poorly understood. Here we report a case of a cecal fecalith encased in mucosa discovered during a routine colonoscopy, concerning for a gastrointestinal stromal tumor (GIST).
Case Description/Methods:
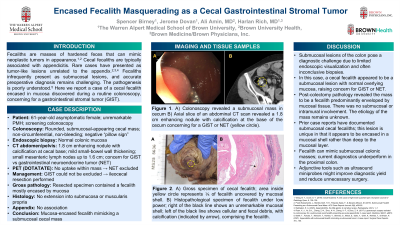
A 61-year-old asymptomatic female with an unremarkable past medical history underwent a screening colonoscopy which identified a rounded submucosal appearing mass in the cecum. The mass was non-circumferential, non-bleeding, and negative for a “pillow sign”. Endoscopic biopsy revealed normal colonic mucosa.
Abdominal CT demonstrated a 1.8 cm enhancing nodule with calcification at the cecal base concerning for a GIST or neuroendocrine tumor (NET). Mild small bowel wall thickening and small mesenteric lymph nodes, up to a maximum of 1.6 cm, were noted. A PET scan showed no evidence of dotatate uptake within the mass, excluding a NET.
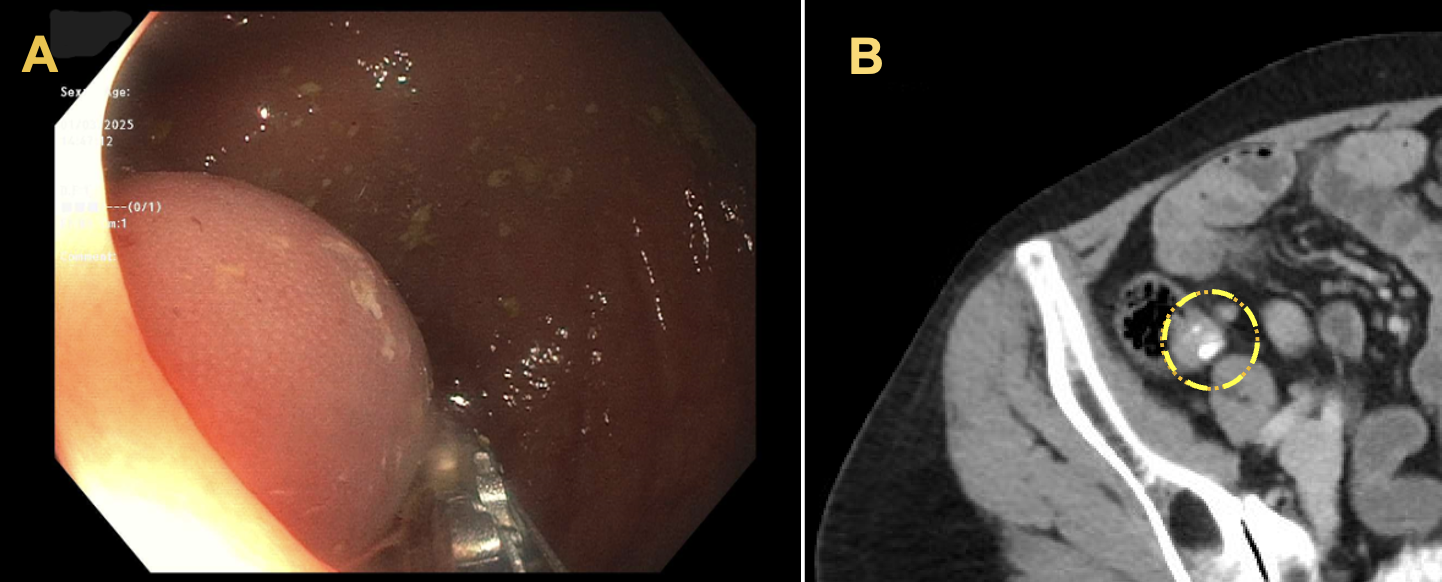
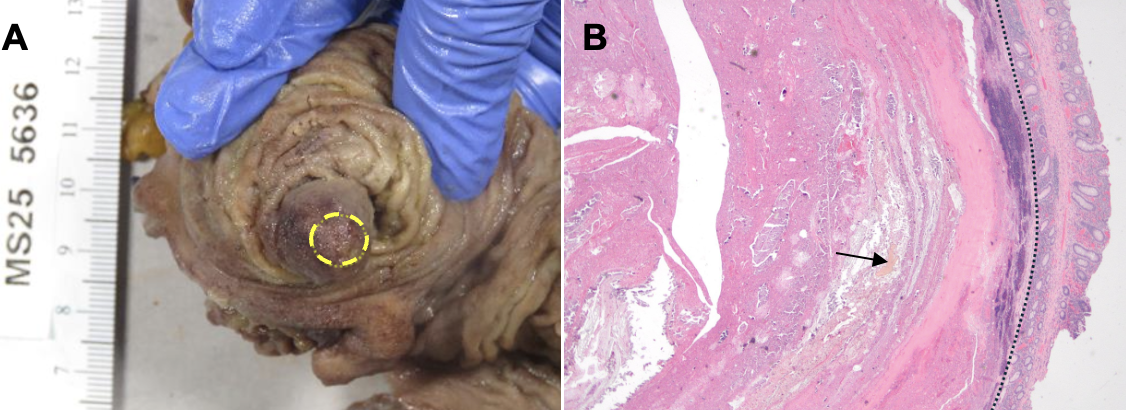
As GIST could not be excluded, the patient underwent ileocecal resection. Macroscopically, the resected specimen revealed a fecalith mostly encased by mucosa. Histology showed no extension into the submucosa or muscularis propria. There was no association with the appendix.
Discussion:
Submucosal lesions of the colon pose a diagnostic challenge due to limited endoscopic visualization and often inconclusive biopsies. In this case, a cecal fecalith appeared to be a submucosal lesion with normal overlying mucosa, raising concern for GIST or NET. Post-colectomy pathology revealed the mass to be a fecalith predominantly enveloped by mucosal tissue. There was no submucosal or intramural involvement. The etiology of the mass remains unknown. While prior case reports have documented submucosal cecal fecaliths, this lesion is unique in that it appears to be encased in a mucosal shell rather than deep to the mucosal layer. This case underscores the need to include fecalith in the differential for submucosal colonic lesions and highlights the limitations of current diagnostic tools, especially for proximal colonic lesions. Adjunctive tools such as ultrasound miniprobes might improve diagnostic yield and reduce unnecessary surgery.
Disclosures:
Spencer Birney, BS1, Jerome Dovan, BS1, Ali Amin, MD2, Harlan G. Rich, MD3. P4723 - Encased Fecalith Masquerading as a Cecal Gastrointestinal Stromal Tumor, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
