Tuesday Poster Session
Category: Colon
P4731 - An Atypical Presentation of Gastrointestinal Stromal Tumor in the Rectum: Diagnostic Challenges and Management


Manasa Ginjupalli, MD
Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
1Brooklyn Hospital Center, Brooklyn, NY; 2The Brooklyn Hospital Center, Brooklyn, NY; 3Rutgers New Jersey Medical School, Brooklyn, NY; 4North Alabama Medical Center, Florence, AL
Introduction: Gastrointestinal stromal tumors (GISTs) are the most common non-epithelial tumors of the gastrointestinal tract. They are most often located in the stomach and small intestine, but are also rarely found in other locations. GISTs are typically diagnosed based on their characteristic histopathological and immunohistochemical features. In some cases, the diagnosis can be challenging due to atypical presentations, especially when tumors occur in uncommon locations. We present a case of a GIST located in the rectum, which exhibited atypical gross examination findings and initially non-diagnostic biopsy results.
Case Description/Methods:
We present a 66-year-old male patient with complex medical history, who was initially admitted for hemorrhagic shock caused by a lower gastrointestinal bleed. A colonoscopy was performed, revealing an ulcerated, non-obstructing large mass in the distal rectum, likely the source of the bleeding. However, the biopsy results were non-diagnostic, showing only regular hyperplastic colonic mucosa. The endoscopic images were highly suspicious for an epithelial tumor, likely colorectal cancer, and the patient was advised to undergo an endoscopic ultrasound (EUS) for further evaluation and biopsy of the mass. Unfortunately, he was lost to follow-up.
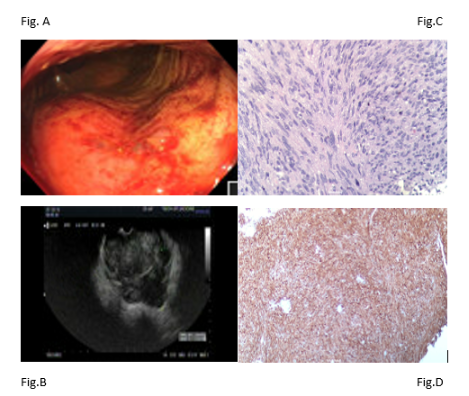
During a subsequent hospital admission for possible ventricular tachycardia, the patient developed another episode of rectal bleeding, likely from the rectal mass. An EUS was performed, which revealed a fungating and ulcerated, non-obstructing large mass in the distal rectum [Fig.A] and fine needle biopsies conducted endo sonographically [Fig.B]. The initial gross findings were suspicious for an epithelial tumor but the surgical pathology revealed a spindle cell neoplasm [Fig.C] , favoring GIST. Immunohistochemical staining was positive for CD117 (c-KIT) [Fig.D], but negative for smooth muscle actin (SMA) and vimentin, confirming the diagnosis.
Given his significant comorbidities, the patient was not considered a surgical candidate. He was referred to oncology, where treatment with imatinib was initiated, and outpatient follow-up was arranged.
Discussion:
GISTs can present in uncommon locations, such as the rectum, and may be challenging to diagnose due to atypical gross findings and non-diagnostic biopsies. It is essential to pursue further evaluation with advanced imaging and immunohistochemistry to ensure an accurate diagnosis and guide appropriate treatment, especially when surgery is not an option.
Disclosures:
Manasa Ginjupalli, MD1, Taranika Sarkar Das, MD2, Sweta Lohani, MD1, Oleksandr Shumeiko, MD2, Hamsika Moparty, MD3, Hima Varsha Voruganti, MD4, Arnold Forlemu, MD1, Jamil Shah, MD2. P4731 - An Atypical Presentation of Gastrointestinal Stromal Tumor in the Rectum: Diagnostic Challenges and Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
