Tuesday Poster Session
Category: Colon
P4604 - Immune Mediated Colitis With Visible Endoscopic Changes and Lymphocytic Histologic Changes: A Diagnostic Conundrum
- JW
Jessica E. Woodham, DO
University of South Alabama
Mobile, AL
Presenting Author(s)
1University of South Alabama, Mobile, AL; 2University of South Alabama College of Medicine, Mobile, AL
Introduction: Immune mediated colitis has become a condition that gastroenterologists must identify and treat as cancer therapy has evolved. Symptoms from immune mediated colitis can be severe. Here we present a case of immune mediated colitis with unexpected endoscopic and pathologic findings.
Case Description/Methods:
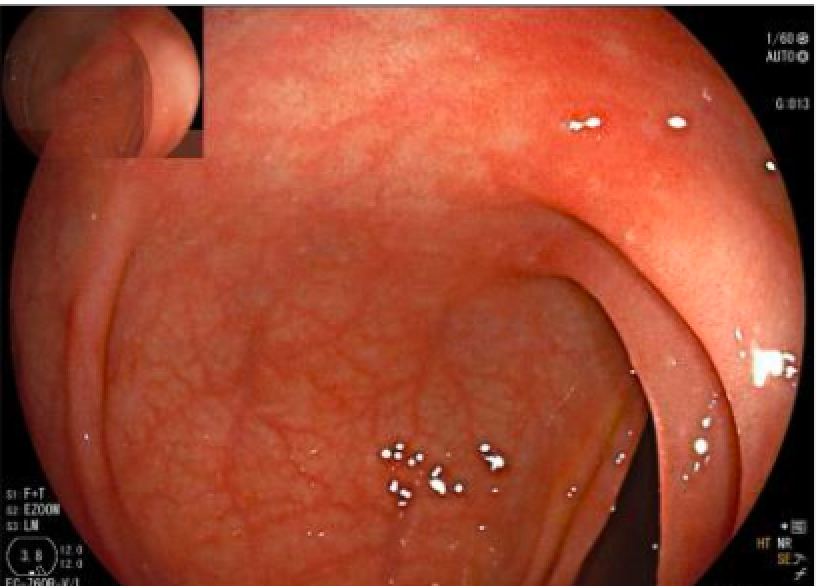
A 61 year old female with invasive ductal carcinoma of the breast was referred to the gastroenterology clinic for evaluation of severe diarrhea. She reported onset of symptoms 3 weeks prior and described watery diarrhea 4 to 5 times per day despite taking loperamide. She denied fever and hematochezia but had some associated abdominal pain and fecal incontinence. She was receiving carboplatin, paclitaxel, and pembrolizumab and last received pembrolizumab one and a half months ago; this regimen was initiated around 3 months prior to presentation. Escitalopram was also started 3 months prior. Infectious stool studies were negative. The patient decided to taper her escitalopram as she did not find it to be efficacious. She was scheduled for a colonoscopy which showed normal terminal ileum but mild patchy colitis in the ascending, transverse, and descending colon. The patient was initiated on controlled ileal release budesonide 9 mg daily. Biopsies revealed lymphocytic colitis throughout the colon. Pembrolizumab was stopped as endoscopic findings were consistent with immune mediated colitis. She noticed rapid improvement in her symptoms after budesonide initiation.
Discussion: Ultimately, this case is unique because there seems to be discordance in the diagnosis based on endoscopic and pathologic findings. Case reports have shown that patients can develop microscopic colitis secondary to use of checkpoint inhibitors, however to our knowledge none of these cases have shown visible changes on endoscopy. Likewise, there are many cases of endoscopically visible changes in immune mediated colitis, however the pathologic findings typically include a mixed cellular inflammatory infiltrate, crypt abscesses or cryptitis. The confounder in this scenario is the use of escitalopram, which is known to cause microscopic colitis. Therefore, this case presents unique endoscopic and pathologic findings incited by checkpoint inhibitor use or concomitant effects from both checkpoint inhibitor use and SSRI use. This case is important in the age of growing checkpoint inhibitor use for cancers and various presentations of immune mediated colitis with potential microscopic colitis overlap.
Disclosures:
Jessica E. Woodham, DO1, William Sonnier, MD2. P4604 - Immune Mediated Colitis With Visible Endoscopic Changes and Lymphocytic Histologic Changes: A Diagnostic Conundrum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
