Monday Poster Session
Category: Stomach and Spleen
P4184 - Assessing Helicobacter pylori Testing and Treatment by Providers at an Academic Tertiary Medical Center: A Quality Improvement Project
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Has Audio

Sirisha Gaddipati, MD
University of Miami Miller School of Medicine
Miami, FL
Presenting Author(s)
Sirisha Gaddipati, MD1, Alejandro Rodriguez, MD, MS2, Ami Panara Shukla, MD3
1University of Miami Miller School of Medicine, Miami, FL; 2University of Miami/ Jackson Memorial Hospital, Hialeah, FL; 3University of Miami Health System, Miami, FL
Introduction: Helicobacter pylori infection (HPI) is one of the most common infections worldwide. In 2018, we started a quality improvement (QI) project at our multihospital urban tertiary care academic center to improve management of HPI. To assess baseline knowledge, in 2018 we performed an IRB approved survey of primary care and GI providers and found 20% were considering serology as a diagnostic option, 50% were treating asymptomatic patients with HPI, 15% were primarily treating with PPI-Bismuth-Metronidazole-Tetracycline (PBMT), 38% were always checking for eradication and 98% said local resistance information for HPI would be helpful. As a result, we had multifold aims including assessing local resistance and improving provider guideline adherence.
Methods: Interventions started in 2018 by collecting prospective culture-based resistance data on a subset of patients with HPI and retrospective analysis of eradication success based on treatment, both suggesting >25% clarithromycin resistance. Educational initiatives included presenting this information at grand rounds for medicine and family medicine departments in 2023 and residency academic lectures in 2025. In 2025, our team created EMR order sets with options for 2 first line medication regimens based on local and national data along with eradication testing orders. From April-May 2025, we sent a 14-question anonymous, IRB approved survey to current residents (medicine-pediatrics, family and internal medicine), primary care and GI providers at our center regarding their HPI management practices.
Results: 108 providers participated in the re-assessment survey (Table 1). Key results include that 8% of providers are using serology for diagnosis, 69% are treating asymptomatic patients with HPI, 81% primarily prescribe PBMT and 78% always tested for eradication (Table 2). 14 % of providers are primarily prescribing PPI-amoxicillin-clarithromycin (PAC).
Discussion: Compared to 2018, 5 times more providers are primarily prescribing PBMT and almost 2 times more are consistently testing for eradication, likely as a result of updated national guidelines and local educational and standardization initiatives. However, 1 in 7 are still primarily prescribing PAC and nearly 1 in 5 are inconsistently ordering eradication testing. Our survey had limited capture of advanced practice providers and attending physicians. Next steps include promoting EMR order set use and reaching out to individual clinics for education.
Disclosures:
Sirisha Gaddipati, MD1, Alejandro Rodriguez, MD, MS2, Ami Panara Shukla, MD3. P4184 - Assessing <i>Helicobacter pylori</i> Testing and Treatment by Providers at an Academic Tertiary Medical Center: A Quality Improvement Project, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Miami Miller School of Medicine, Miami, FL; 2University of Miami/ Jackson Memorial Hospital, Hialeah, FL; 3University of Miami Health System, Miami, FL
Introduction: Helicobacter pylori infection (HPI) is one of the most common infections worldwide. In 2018, we started a quality improvement (QI) project at our multihospital urban tertiary care academic center to improve management of HPI. To assess baseline knowledge, in 2018 we performed an IRB approved survey of primary care and GI providers and found 20% were considering serology as a diagnostic option, 50% were treating asymptomatic patients with HPI, 15% were primarily treating with PPI-Bismuth-Metronidazole-Tetracycline (PBMT), 38% were always checking for eradication and 98% said local resistance information for HPI would be helpful. As a result, we had multifold aims including assessing local resistance and improving provider guideline adherence.
Methods: Interventions started in 2018 by collecting prospective culture-based resistance data on a subset of patients with HPI and retrospective analysis of eradication success based on treatment, both suggesting >25% clarithromycin resistance. Educational initiatives included presenting this information at grand rounds for medicine and family medicine departments in 2023 and residency academic lectures in 2025. In 2025, our team created EMR order sets with options for 2 first line medication regimens based on local and national data along with eradication testing orders. From April-May 2025, we sent a 14-question anonymous, IRB approved survey to current residents (medicine-pediatrics, family and internal medicine), primary care and GI providers at our center regarding their HPI management practices.
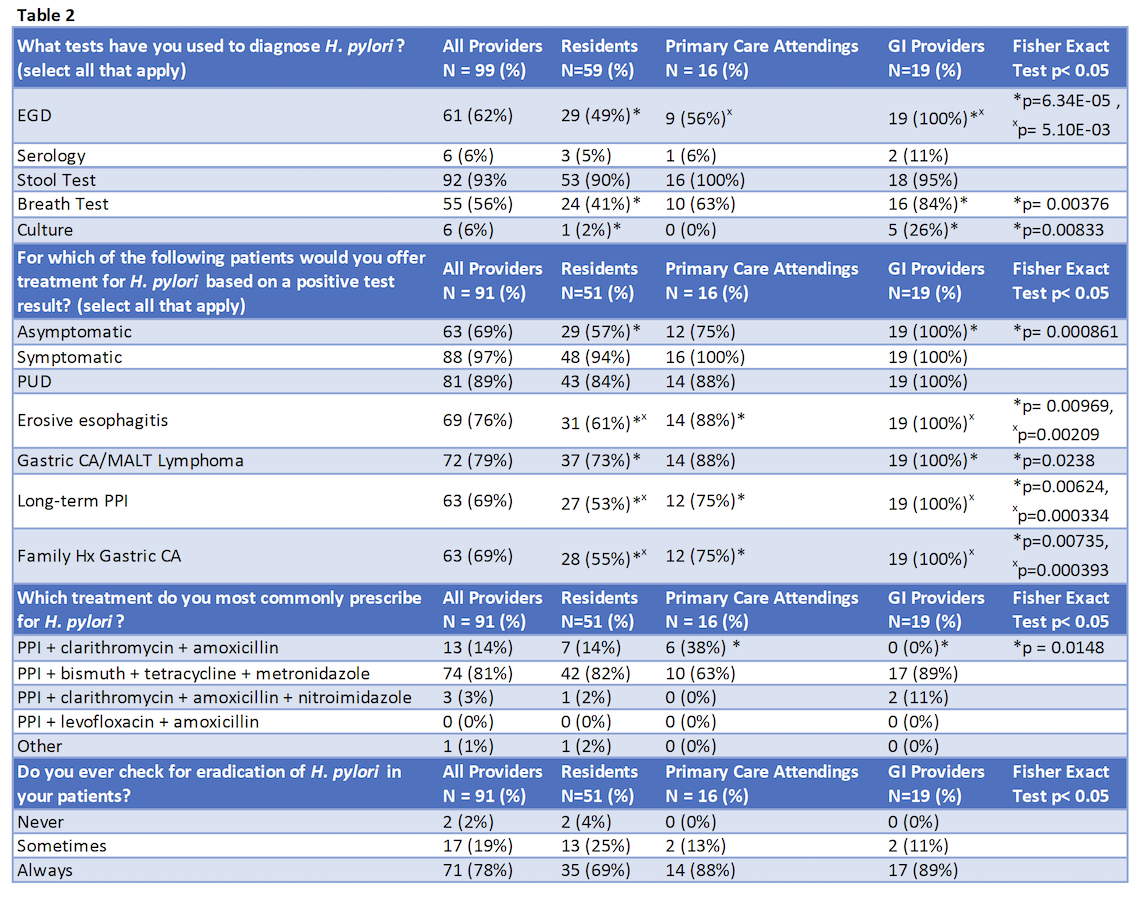
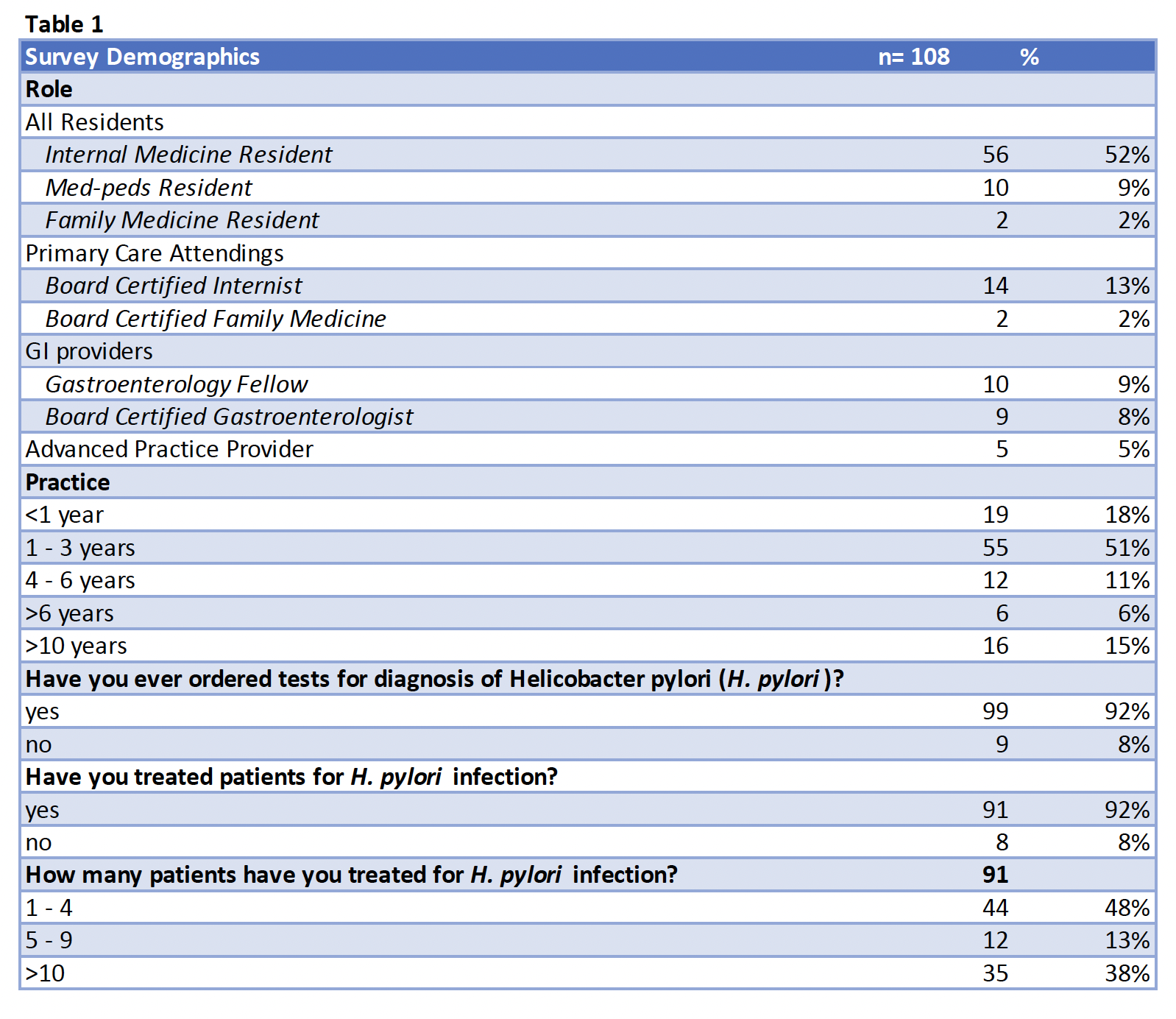
Results: 108 providers participated in the re-assessment survey (Table 1). Key results include that 8% of providers are using serology for diagnosis, 69% are treating asymptomatic patients with HPI, 81% primarily prescribe PBMT and 78% always tested for eradication (Table 2). 14 % of providers are primarily prescribing PPI-amoxicillin-clarithromycin (PAC).
Discussion: Compared to 2018, 5 times more providers are primarily prescribing PBMT and almost 2 times more are consistently testing for eradication, likely as a result of updated national guidelines and local educational and standardization initiatives. However, 1 in 7 are still primarily prescribing PAC and nearly 1 in 5 are inconsistently ordering eradication testing. Our survey had limited capture of advanced practice providers and attending physicians. Next steps include promoting EMR order set use and reaching out to individual clinics for education.
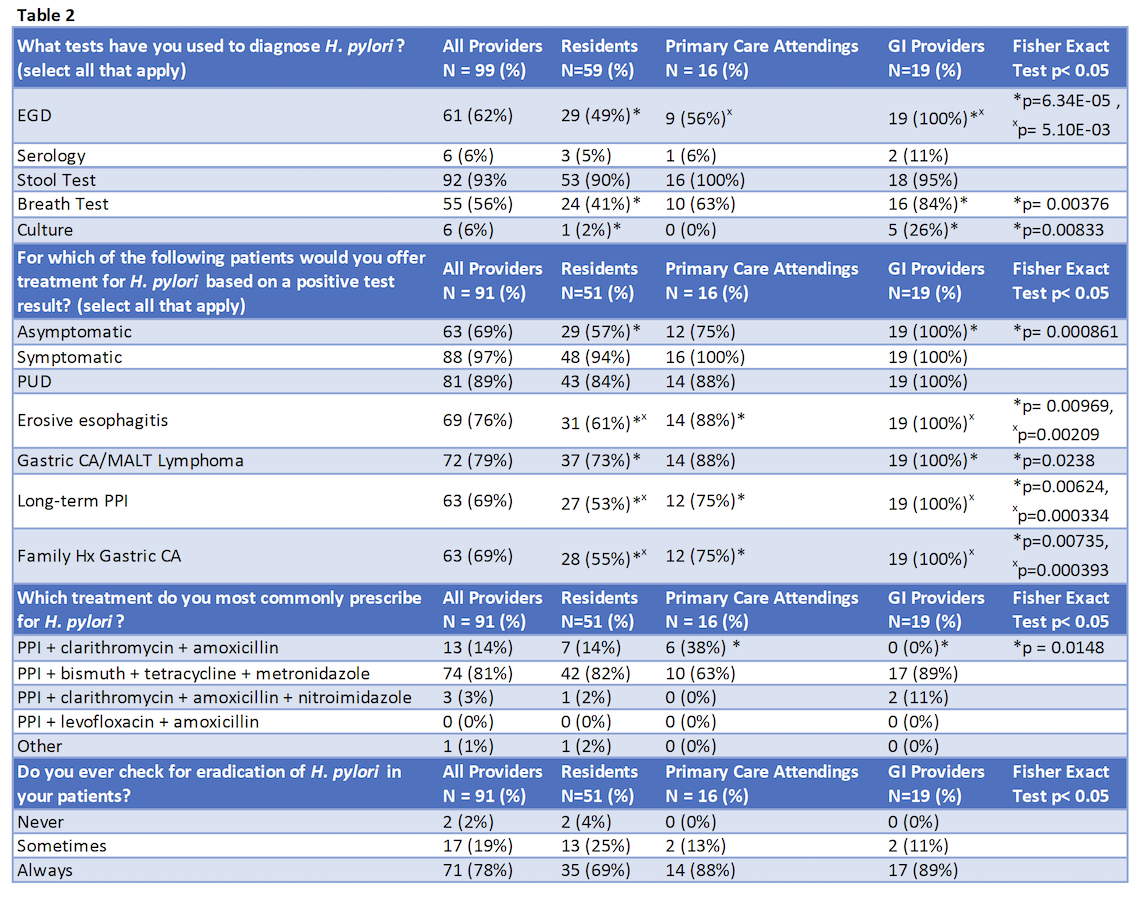
Figure: Table 1. Characteristics of survey participants. Participants were providers in varying roles/training and invited across our multi-hospital urban tertiary care academic center.
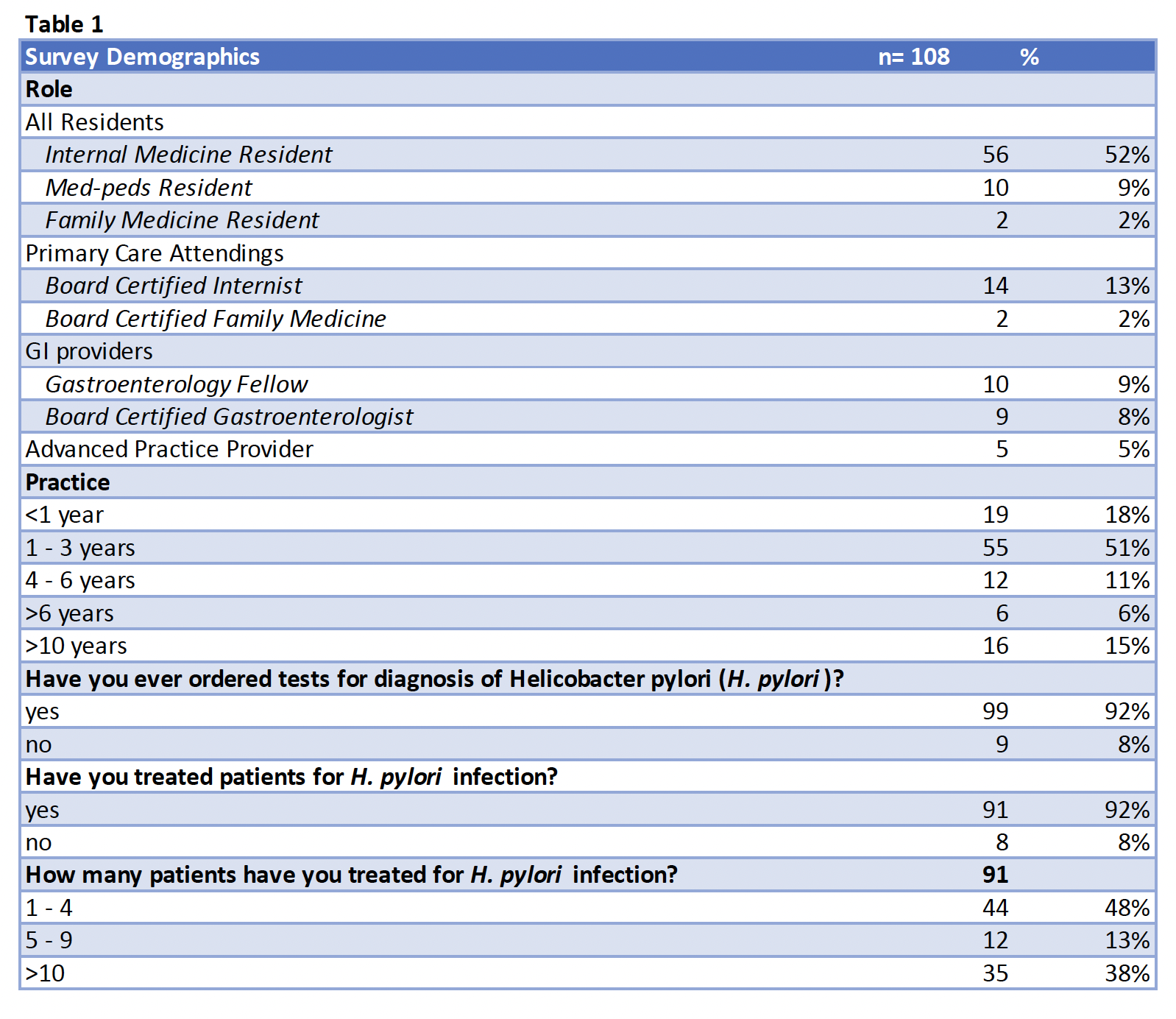
Figure: Table 2. Management of Helicobacter pylori infection by Survey Participants. Results of all providers participating in the survey and by provider role (all residents, primary care attending physicians, GI providers). Statistical analysis performed using Fisher's exact test and Bonferroni correction. P-values provided where adjusted p<0.05 for pairwise comparisons.
Disclosures:
Sirisha Gaddipati indicated no relevant financial relationships.
Alejandro Rodriguez indicated no relevant financial relationships.
Ami Panara Shukla indicated no relevant financial relationships.
Sirisha Gaddipati, MD1, Alejandro Rodriguez, MD, MS2, Ami Panara Shukla, MD3. P4184 - Assessing <i>Helicobacter pylori</i> Testing and Treatment by Providers at an Academic Tertiary Medical Center: A Quality Improvement Project, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
