Monday Poster Session
Category: Colon
P2544 - More Than Just a Gut Feeling: Unmasking Systemic Mastocytosis Behind Chronic GI Symptoms
Grace C. Ramirez, MD
Baycare Health Systems, St. Joseph's Hospital
Tampa, FL
Presenting Author(s)
1Baycare Health Systems, St. Joseph's Hospital, Tampa, FL; 2BayCare Health Systems, St. Joseph’s Hospital, Tampa, FL
Introduction: Systemic mastocytosis is a rare clonal disorder characterized by abnormal proliferation and accumulation of mast cells in multiple organs. Unlike cutaneous mastocytosis, which is confined to the skin, systemic involvement leads to a broad spectrum of symptoms. Gastrointestinal manifestations are common but often non-specific, mimicking other GI disorders and contributing to delayed or missed diagnoses. Early recognition is essential, as symptoms can significantly impact quality of life. We present a case of a 66-year-old woman with debilitating GI symptoms found to be a result of systemic mastocytosis
Case Description/Methods:
A 66-year-old woman with a history of hypertension, GERD, Barrett’s esophagus, and osteoporosis presented with decades-long gastrointestinal symptoms, including abdominal pain, bloating, nausea, vomiting, and diarrhea. Symptoms were intermittently triggered by foods such as alcohol and certain breads and seasonings but sometimes occurred spontaneously with nighttime awakenings. An elimination diet failed to identify consistent triggers and workups for common GI disorders, including celiac disease, were unremarkable.
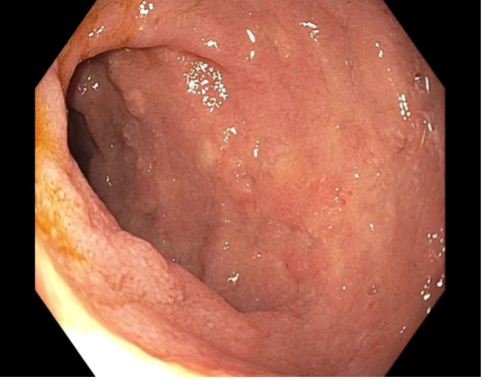
Endoscopic evaluation revealed duodenitis and colitis with histologic features raising suspicion for systemic mastocytosis with CD117+ for mast cells. A bone marrow biopsy later reinforced the diagnosis, demonstrating an activating KIT mutation. Tryptase levels were persistently elevated ( >20 ng/mL). These findings fulfilled both the major and minor diagnostic criteria for systemic mastocytosis, specifically the indolent variant.
After trials with multiple medications, the patient’s symptoms have been controlled with fexofenadine, montelukast, and famotidine. Other medications included Cromolyn, which was discontinued due to poor adherence, and a trial drug, Avapritinib, which was stopped due to lower extremity edema and weight gain.
Discussion: This case illustrates the diagnostic and therapeutic challenges of GI involvement in systemic mastocytosis. Early diagnosis enables targeted management with a multidisciplinary team and can significantly improve outcomes and quality of life. A low-histamine diet, escalated antihistamine therapy, and consideration of advanced therapies may also provide symptomatic relief and improve quality of life.

Disclosures:
Grace Ramirez, MD1, Yesenia Gonzalez, MD1, Antoine Khoudari, MD1, Ashley H. Davis-Yadley, MD2. P2544 - More Than Just a Gut Feeling: Unmasking Systemic Mastocytosis Behind Chronic GI Symptoms, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
