Monday Poster Session
Category: Colon
P2547 - Colonic Kaposi Sarcoma Masquerading as Infectious Colitis in a Patient With AIDS
- VR
Vaibhav Rastogi, MD
Medical College of Georgia at Augusta University
Augusta, GA
Presenting Author(s)
Danny Alevy, BS, Dipen Mehta, , Robert VanBrackle Jr, , Hrithik Dakssesh Putta Nagarajan, MBBS, Vaibhav Rastogi, MD, Amanda Barrett, MD, Viveksandeep Thoguluva Chandrasekar, MBBS
Medical College of Georgia at Augusta University, Augusta, GA
Introduction:
Kaposi sarcoma (KS) is a vascular endothelial neoplasm associated with human herpesvirus 8 (HHV-8), predominantly occurring in immunocompromised individuals, recognized as an AIDS-defining illness. In the context of ongoing AIDS, infectious colitis can complicate the differential diagnosis. Overlapping symptoms of potential colonic pathologies may lead to missed diagnoses and delayed treatment, which is particularly concerning given the high acuity and mortality associated with conditions such as KS. We present a patient with AIDS who was diagnosed with colonic KS in the context of infectious colitis.
Case Description/Methods:
A 34-year-old male with history of advanced HIV with non-compliance to antiretroviral therapy (ART), KS with cutaneous, pulmonary, and osseous involvement, s/p four cycles of doxorubicin and paclitaxel, anal intraepithelial neoplasia treated via surgical excision, pulmonary embolism on apixaban presented to the hospital with a four-day history of diffuse abdominal pain accompanied by a one-day history of hematochezia.
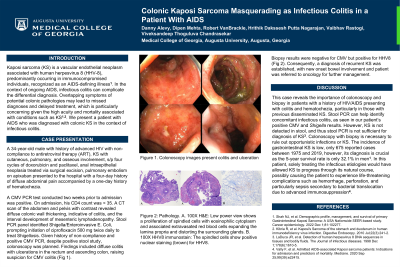
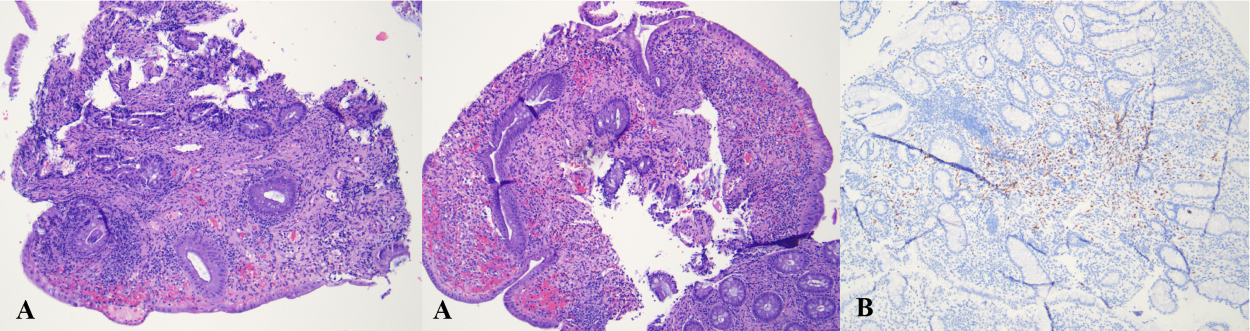
A CMV PCR test conducted two weeks prior to admission was positive. On admission, his CD4 count was < 35. A CT scan of the abdomen and pelvis with contrast revealed diffuse colonic wall thickening, indicative of colitis, and the interval development of mesenteric lymphadenopathy. Stool PCR panel identified Shigella/Enteroinvasive E. coli, prompting initiation of ciprofloxacin 500 mg twice daily to treat shigellosis. Given history of non-compliance and positive CMV PCR, despite positive stool study, colonoscopy was planned. Findings included diffuse colitis with ulcerations in the rectum and ascending colon, raising suspicion for CMV colitis (Fig 1). Biopsy results were negative for CMV but positive for HHV8 (Fig 2). Consequently, a diagnosis of recurrent KS was established, with new onset bowel involvement and patient was referred to oncology for further management.
Discussion: This case underscores the critical role of colonoscopy and biopsy in patients with a history of HIV/AIDS who present with colitis and hematochezia. While a stool PCR panel is beneficial for excluding concomitant infectious colitis, a high index of suspicion is necessary for other etiologies in the appropriate clinical context. Colonoscopy with biopsy is essential to exclude opportunistic infections or KS. The incidence of gastrointestinal KD is low, only 675 reported cases between 1975 and 2019, however, its diagnosis is crucial as the 5-year survival rate is only 32.1% in men.
Disclosures:
Danny Alevy, BS, Dipen Mehta, , Robert VanBrackle Jr, , Hrithik Dakssesh Putta Nagarajan, MBBS, Vaibhav Rastogi, MD, Amanda Barrett, MD, Viveksandeep Thoguluva Chandrasekar, MBBS. P2547 - Colonic Kaposi Sarcoma Masquerading as Infectious Colitis in a Patient With AIDS, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

