Monday Poster Session
Category: Colon
P2553 - Cronkhite-Canada Syndrome: A Rare Constellation of Intestinal Polyposis and Dermatologic Abnormalities


Christina Joya, DO
Valley Hospital Medical Center
Las Vegas, NV
Presenting Author(s)
1Valley Hospital Medical Center, Las Vegas, NV; 2Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV
Introduction: Cronkhite-Canada Syndrome (CCS) is a rare acquired syndrome characterized by gastrointestinal polyposis, alopecia, nail atrophy, skin hyperpigmentation, and diarrhea resulting in malabsorption. CCS has an estimated incidence of one case per million people, with approximately five hundred total reported cases. We report a case of CCS in an elderly female with chronic diarrhea - one of few cases reported in the United States.
Case Description/Methods:
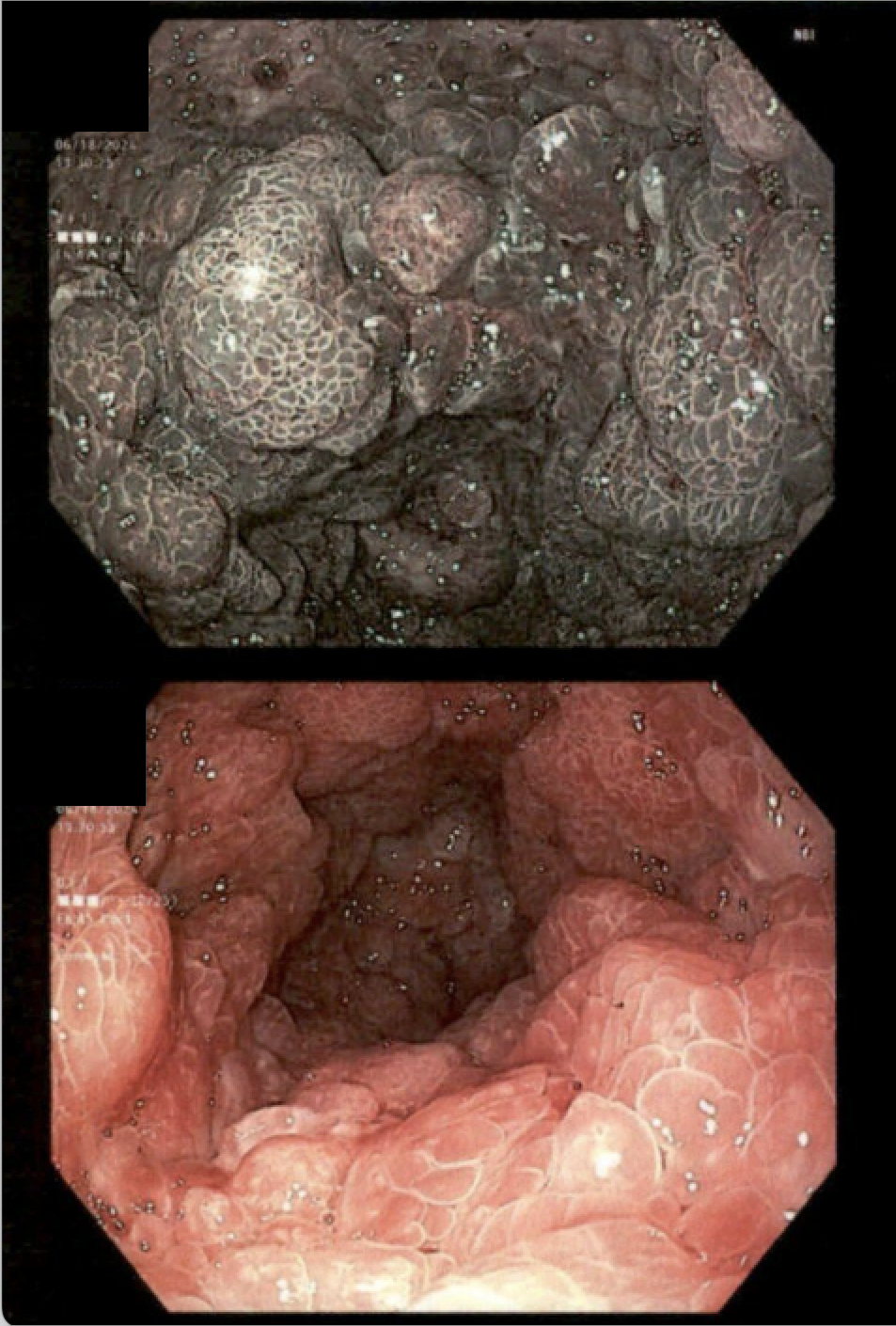
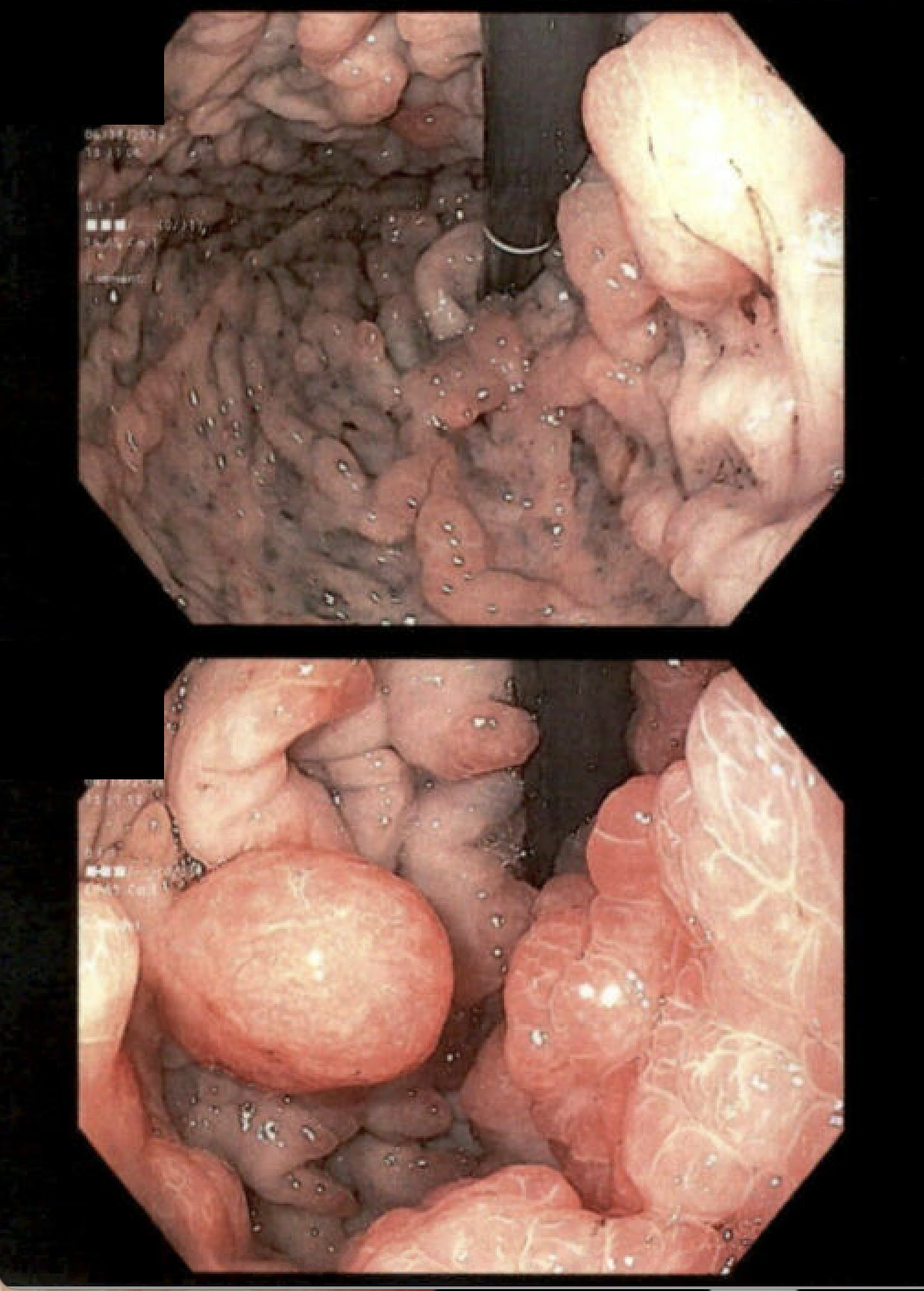
A 79-year-old Asian female with hypothyroidism presented with four months of profuse watery diarrhea (up to 10 episodes/day), generalized weakness, and a 20-lb unintentional weight loss over six months. Laboratory evaluation revealed hemoglobin 8.8 g/dL, platelet count 884K, sodium 120 mmol/L, and potassium 3.4 mmol/L. C. difficile PCR was negative. EGD showed enlarged gastric folds with edema, friability, and nodularity. The duodenum was carpeted with polyps, including a large pedunculated lesion in the proximal sweep. Colonoscopy revealed innumerable subcentimeter sessile polyps, colitis, and mucosal erythema. Biopsies were consistent with inflammatory polyps. CEA was mildly elevated (11.2 ng/mL). She tested positive for Helicobacter pylori and was treated accordingly.
The patient also exhibited alopecia, hyperpigmented rash, and onychodystrophy. Further workup for malabsorptive and autoimmune etiologies was unremarkable. Based on the constellation of GI and ectodermal findings, CCS was diagnosed. She relocated to Singapore where she was started on azathioprine and prednisolone. Upon return to the U.S., worsening malnutrition, non-healing sacral wounds, and multiple pathologic fractures necessitated TPN. Due to persistent symptoms, escalation to biologics was considered, but she ultimately opted for palliative care.
Discussion:
The etiology of CCS remains unclear. Physical stress, autoimmune tendencies, H. pylori infection, and allergic response (particularly to oral thyroxine, which our patient was on for hypothyroidism) have been hypothesized to contribute to the development of CCS. Patients with CCS typically present with hyperpigmented skin, alopecia, nail changes, and chronic diarrhea with malnutrition. Endoscopy often shows hamartomatous and inflammatory polyps, giant mucosal folds, and mucosal edema. Treatment involves steroids, immunosuppressives, and biologics, though no standardized regimen exists. Prognosis is poor with a 5-year survival rate under 45%. Early diagnosis and intervention may improve outcomes.
Disclosures:
Christina Joya, DO1, Zurriat Syed, DO2, Masuma Syed, MD1, Scott Silver, DO1, Vishvinder Sharma, MD1. P2553 - Cronkhite-Canada Syndrome: A Rare Constellation of Intestinal Polyposis and Dermatologic Abnormalities, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
