Monday Poster Session
Category: Colon
P2465 - A Diagnostic Odyssey: Enterocolic Lymphocytic Phlebitis Presenting as Refractory Colitis

John Thesing, DO
University of Kansas School of Medicine - Wichita
Wichita, KS
Presenting Author(s)
1University of Kansas School of Medicine - Wichita, Wichita, KS; 2University of Kansas School of Medicine, Wichita, KS
Introduction:
Case Description/Methods:
A 74-year-old male with coronary artery disease presented with abdominal pain, diarrhea, and anorexia for one week. He had multiple ED visits; each time he was discharged home with pain medication and antibiotics. Computed tomography (CT) scans revealed nonspecific, left-sided colitis.
He represented with worsening abdominal pain, bloody diarrhea, and fever. CT showed recto-colitis and new ascites. Inflammatory markers were elevated: erythrocyte sediment rate 27 mm/hr and c-reactive protein 27.2 mg/dL. Fecal calprotectin was normal at 9 mcg/g. Infectious stool PCR was negative. Symptoms progressed despite broad spectrum antibiotics.
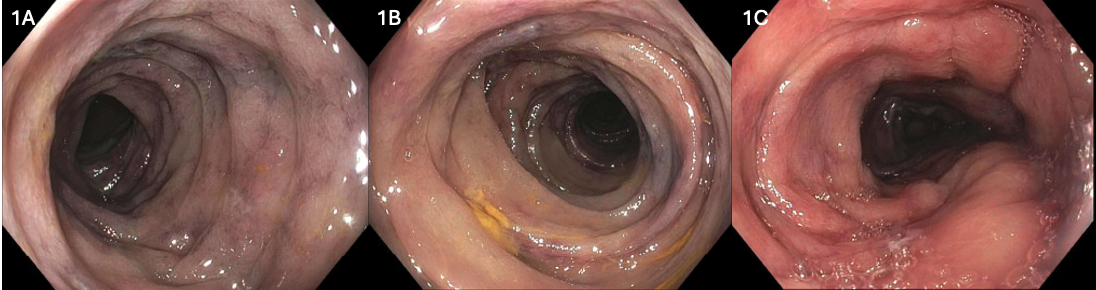
Flexible sigmoidoscopy revealed severely congested and edematous mucosa in the rectum, sigmoid, and descending colon without ulceration or overt inflammation (Figure 1). Findings raised concern for venous congestion. On pathology, active colitis was not seen; the mucosa was intact but there was scattered vascular microthrombi and hyalinized stroma suggestive of ischemic changes. Abdominal CT venogram to rule out ischemic and venous thrombotic disease involving the venous system was pursued. There was redemonstration of proctocolitis, increased ascites, and prominent left-sided pericolonic veins, suspicious for idiopathic myointimal hyperplasia of the mesenteric veins (Figure 2).
Curative treatment is surgery and with worsening symptoms surgery was performed. Intraoperatively, dense inflammation precluded a full resection, and a diverting loop colostomy was completed. Intraoperative mesenteric biopsies revealed ELP. Four months later, he underwent a successful hemicolectomy with hartman’s pouch and permanent end colostomy.
Discussion:
This case highlights the diagnostic complexity of ELP, a rare and underrecognized cause of colitis. Given his venous thrombosis, hypercoagulable testing was performed and showed heterozygous Factor V Leiden. The nonspecific findings often mimic common conditions, delaying diagnosis. A multimodal approach, including CT venography and endoscopy, guided timely surgical intervention. The presence of Factor V Leiden may suggest a prothrombotic component and warrants further investigation.

Disclosures:
John Thesing, DO1, Meagan H. Phox, DO2, Hasan Jaber, MD2, Kevin Singh, MD2, Kyle Rowe, MD2. P2465 - A Diagnostic Odyssey: Enterocolic Lymphocytic Phlebitis Presenting as Refractory Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
