Monday Poster Session
Category: Colon
P2470 - Primary Colonic DLBCL in a Young Incarcerated Male: A Diagnostic Pitfall Highlighting Health Disparities

Muhammad Sohaib Alvi, MBBS, MD
Ascension Saint Joseph Hospital
Chicago, IL
Presenting Author(s)
1Ascension Saint Joseph Hospital, Chicago, IL; 2Saint Joseph medical center, Plainfield, IL; 3St. Joseph's Medical Centre, Joliet, IL; 4saint joseph medical centre, Joliet, IL; 5Prime Health SJMC, Lockport, IL; 6Wright Center for Graduate Medical Education, Scranton, PA
Introduction:
Primary colonic diffuse large B-cell lymphoma (DLBCL) is a rare gastrointestinal malignancy, accounting for less than 1% of GI lymphomas. Frequently misdiagnosed as adenocarcinoma, it leads to diagnostic delays and inappropriate management. We report a case of obstructive colonic DLBCL in a young incarcerated male, emphasizing diagnostic challenges, healthcare disparities, and the need for timely multidisciplinary care.
Case Description/Methods:
A 32-year-old incarcerated male with GERD and prior appendectomy presented with three months of intermittent right lower quadrant pain, hematochezia, and vomiting. An off-site CT scan arranged by correctional health services three weeks prior revealed a 10.3 cm ascending colon mass, yet colonoscopy was delayed due to limited facility resources. Upon worsening symptoms, he was transferred to the emergency department with stable vital signs (BP 126/70, HR 82) and severe right lower quadrant tenderness. Rectal exam revealed maroon stool. Labs showed hemoglobin 7.0 g/dL and mean corpuscular volume 68 fL. Carcinoembryonic antigen (CEA) was normal at 1.2 ng/mL. A repeat CT showed rapid tumor growth to 14 cm, small bowel obstruction, and right hydronephrosis. Colonoscopy confirmed a large, ulcerated, obstructive mass, with deep biopsies revealing CD20-positive, CD10-positive lymphoid cells and a Ki-67 index >90%. He underwent emergent right hemicolectomy with negative surgical margins. Pathology confirmed DLBCL without bone marrow involvement or MYC, BCL2, or BCL6 rearrangements. He commenced chemotherapy promptly with R-CHOP following oncology consultation.
Discussion:
This case highlights critical diagnostic considerations for differentiating colonic DLBCL from adenocarcinoma, emphasizing atypical features including young age, rapid mass growth, and normal CEA levels. Deep biopsies are essential due to the submucosal nature of lymphoma lesions that superficial biopsies might miss. Moreover, this report clearly illustrates how healthcare disparities within correctional facilities contributed directly to significant diagnostic delays, potentially worsening outcomes given lymphoma's rapid progression and potentially fatal nature if untreated. Implementing standardized timelines for cancer screening and expedited specialist access in correctional settings could substantially improve patient outcomes.
Formatting support was provided using an AI tool under the author's supervision, in accordance with ACG guidelines.
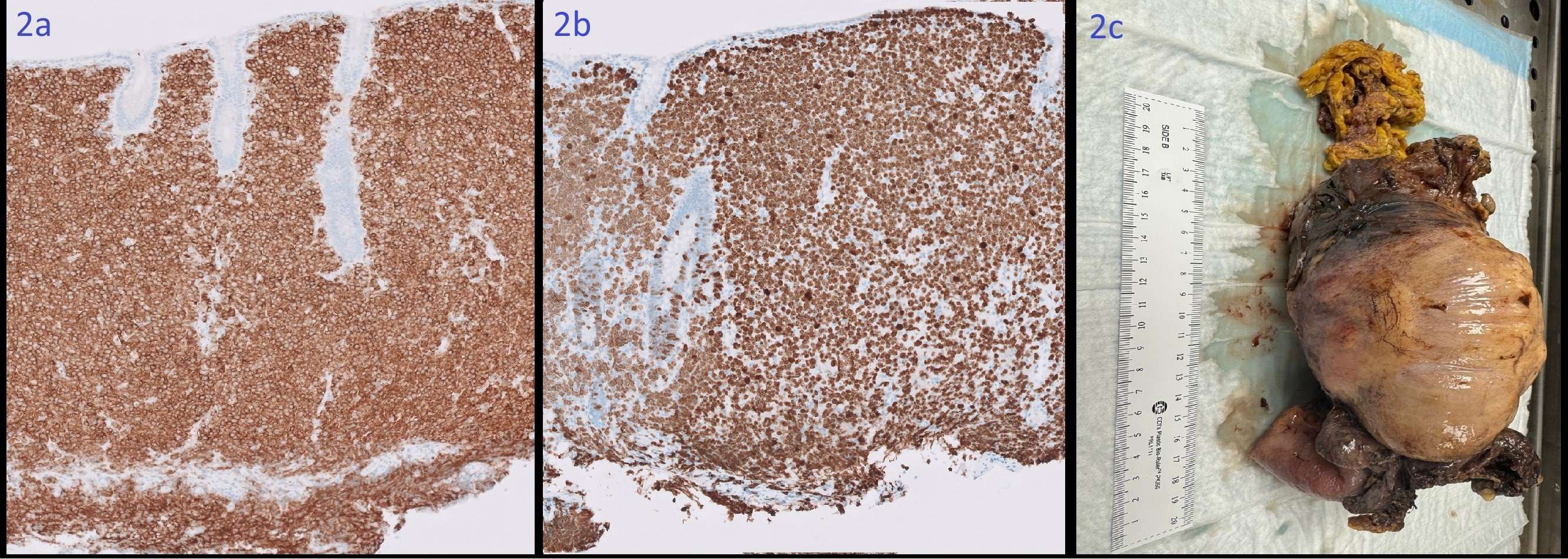
Figure 1b: Colonoscopy image demonstrating a large, smooth, well-circumscribed, submucosal mass lesion with an intact overlying mucosa in the proximal colon
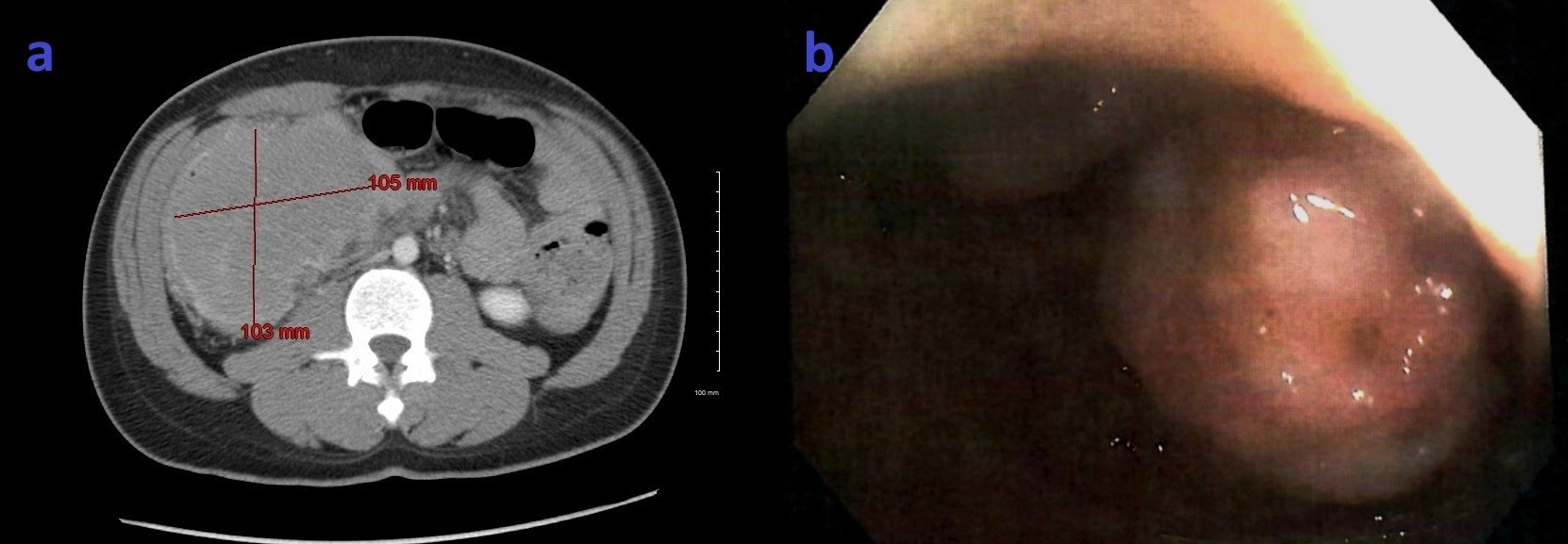
Figure 2b: Immunostain for Ki-67 highlights greater than 90% of the malignant cells.
Figure 2c: Gross right hemicolectomy specimen showing a 14 cm exophytic colonic mass.
Disclosures:
Muhammad Sohaib Alvi, MBBS, MD1, Yasmin Gerais, MBBS, MD2, Bachar Hamad, MD3, Anas Mahmoud, MD4, Mohamed Boshnaf, MD, MPH5, Ebram Said, MD1, Mohamed A. Ebrahim, MD1, Ashok Kumar, MD1, Sunny Kumar, MD6. P2470 - Primary Colonic DLBCL in a Young Incarcerated Male: A Diagnostic Pitfall Highlighting Health Disparities, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
