Monday Poster Session
Category: Colon
P2532 - A Case Report of Clostridium perfringens Bacteremia Following Colorectal Cancer Resection

Mena Saad, DO
Riverside University Health System
Moreno Valley, CA
Presenting Author(s)
1Riverside University Health System, Moreno Valley, CA; 2Riverside University Health System, Loma Linda, CA; 3The Ohio State University Wexner Medical Center, Columbus, OH; 4Riverside University medical center, Moreno Valley, CA
Introduction:
The association between clostridial bacteremia and colorectal cancer is well documented in the literature. In particular, Clostridium perfringens bacteremia often warrants further evaluation for an underlying malignancy, such as colorectal cancer. Here, we present a case of a patient who developed C. perfringens bacteremia several months after undergoing resection for colorectal cancer.
Case Description/Methods:
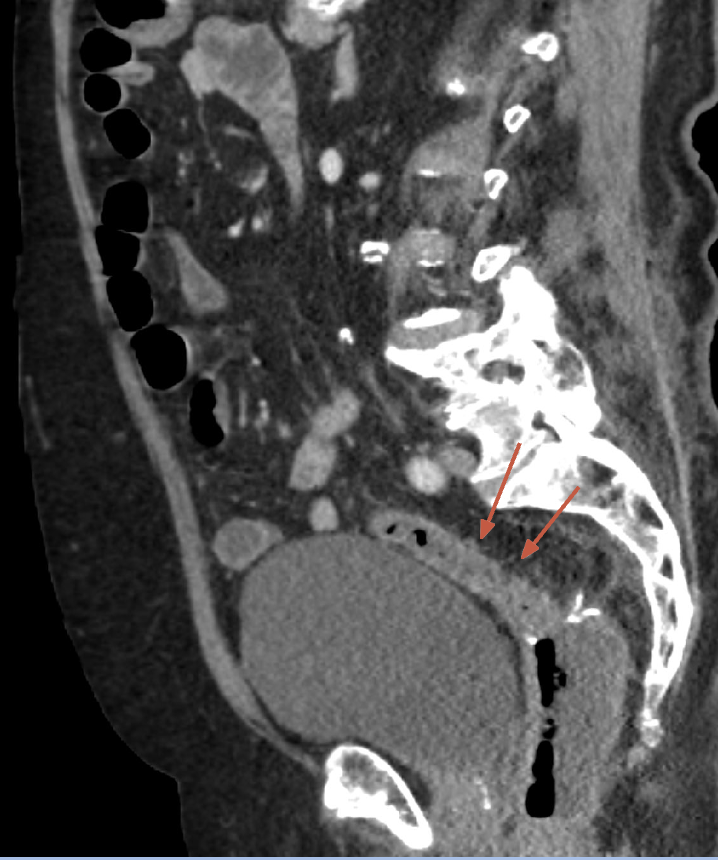
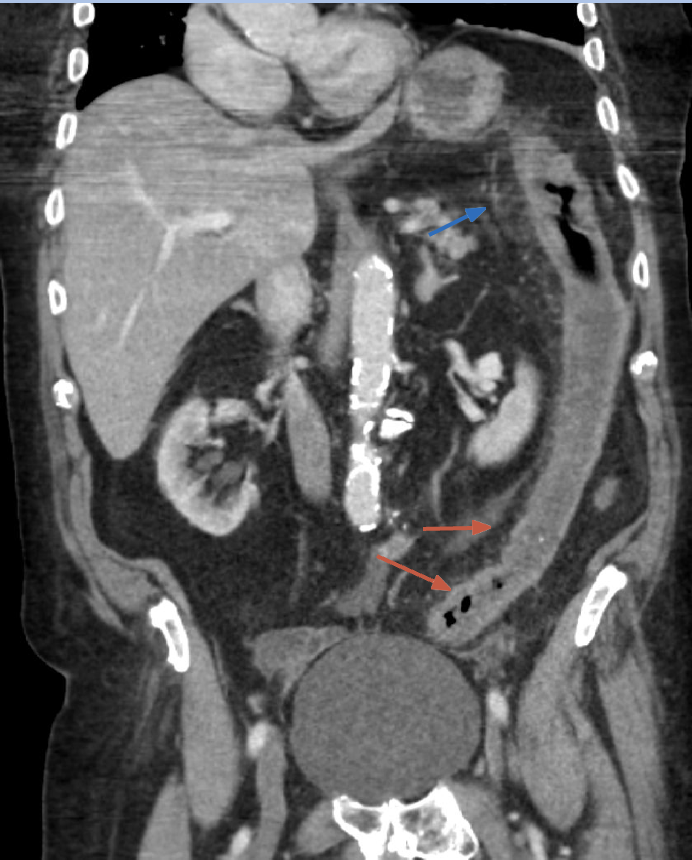
An 81-year-old male presented to the hospital with recent worsening symptoms of intermittent diarrhea in the last months. Past medical history was notable for prostate cancer in remission and colon cancer status post resection of a fungating and ulcerated partially obstructing mass in the recto-sigmoid colon 6 months before presentation. Initial laboratory findings were significant for a white blood cell count of 13.3 g/dL. Physical exam was notable for mild diffuse abdominal tenderness. CT abdomen and pelvis revealed colitis in the distal transverse colon, descending colon, and sigmoid colon without obstruction. Blood cultures were significant for Clostridium Perfringens in one of two blood cultures. Infectious Disease was consulted and recommended treatment with ampicillin-sulbactam with the transition to oral amoxicillin-clavulanate upon discharge. Blood cultures were repeated and were found to be negative. The patient's diarrhea improved. The etiology of the C. perfringens bacteremia was suspected to be due to gut translocation from recent colon surgery.
Discussion:
Clostridium perfringens bacteremia, though relatively rare overall, is notably more common in individuals with colorectal cancer. Multiple retrospective studies have established a strong association between colorectal malignancies and C. perfringens bacteremia, highlighting the need for careful evaluation of gastrointestinal cancers in affected patients. However, this condition is infrequent in patients who are in remission. Risk factors for its development include malignancies—particularly colorectal and hepatobiliary cancers—renal insufficiency, and immunosuppression, such as neutropenia following chemotherapy. Recent colorectal surgery can also contribute by altering gut microbiota and causing dysbiosis, potentially leading to colitis and bacteremia. Early recognition and prompt initiation of appropriate antibiotic therapy are essential for improving outcomes.
Disclosures:
Mena Saad, DO1, Julia M. Gomez, MD2, Medora Doris. Rodrigues, MD, MPH3, Matthew Orosa, DO1, Huy Au, MD1, Lakshmi K. Puvvula, MD4, Steve Serrao, MD1. P2532 - A Case Report of <i>Clostridium perfringens</i> Bacteremia Following Colorectal Cancer Resection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
