Sunday Poster Session
Category: Infections and Microbiome
P1309 - Declining Mortality From Clostridioides difficile Infection Following Therapeutic Innovation: A 25-Year National Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Has Audio

George S. Blewusi, MD
Johns Hopkins Bloomberg School of Public Health
Baltimore, MD
Presenting Author(s)
John K. Appiah, MD1, George S. Blewusi, MD2, Richeal Asante, MD3, Emmanuel Asare, 4, John Boger, MD1
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 3Geisinger Wyoming Valley Medical Center, Kingston, PA; 4Montefiore hospital, Bronx, NY
Introduction: The introduction of fidaxomicin, bezlotoxumab, and fecal microbiota-based therapies marks a new era in the management of Clostridioides difficile infection (CDI). However, the impact of these therapeutic advances on population-level CDI-associated mortality remains unclear. This study evaluates national trends in CDI mortality before and after their introduction, with secondary analyses by age group and geographic setting.
Methods: CDC WONDER Multiple Cause of Death data (1999–2023) were used to identify all deaths listing CDI as a cause. Crude mortality rates per 100,000 population were calculated annually and summarized in five-year intervals. The post-therapeutic era was defined as beginning in 2011, corresponding to the approval of fidaxomicin. Mortality was further stratified by five-year age groups and urban-rural status using the 2013 NCHS Urban-Rural Classification.
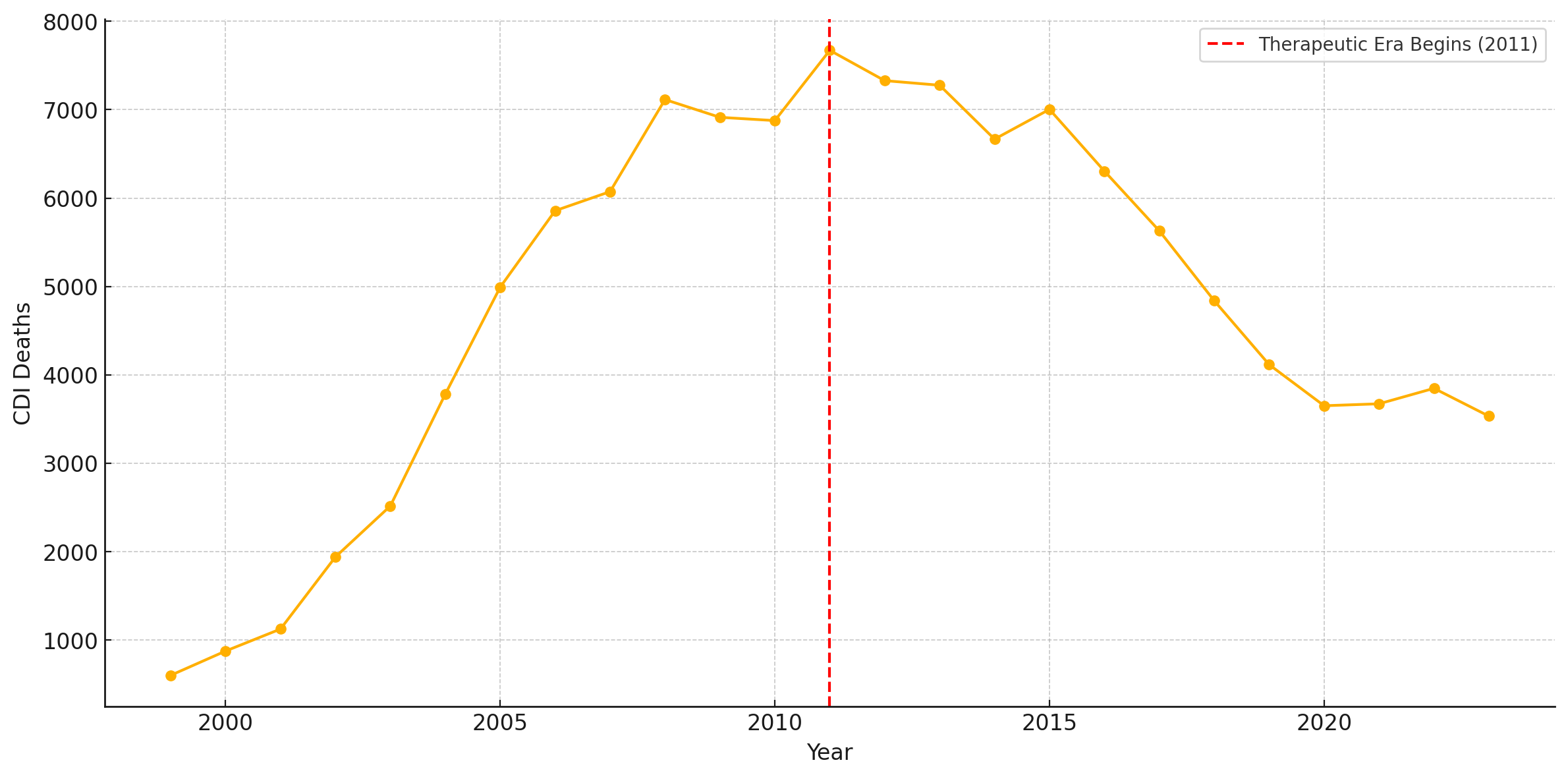
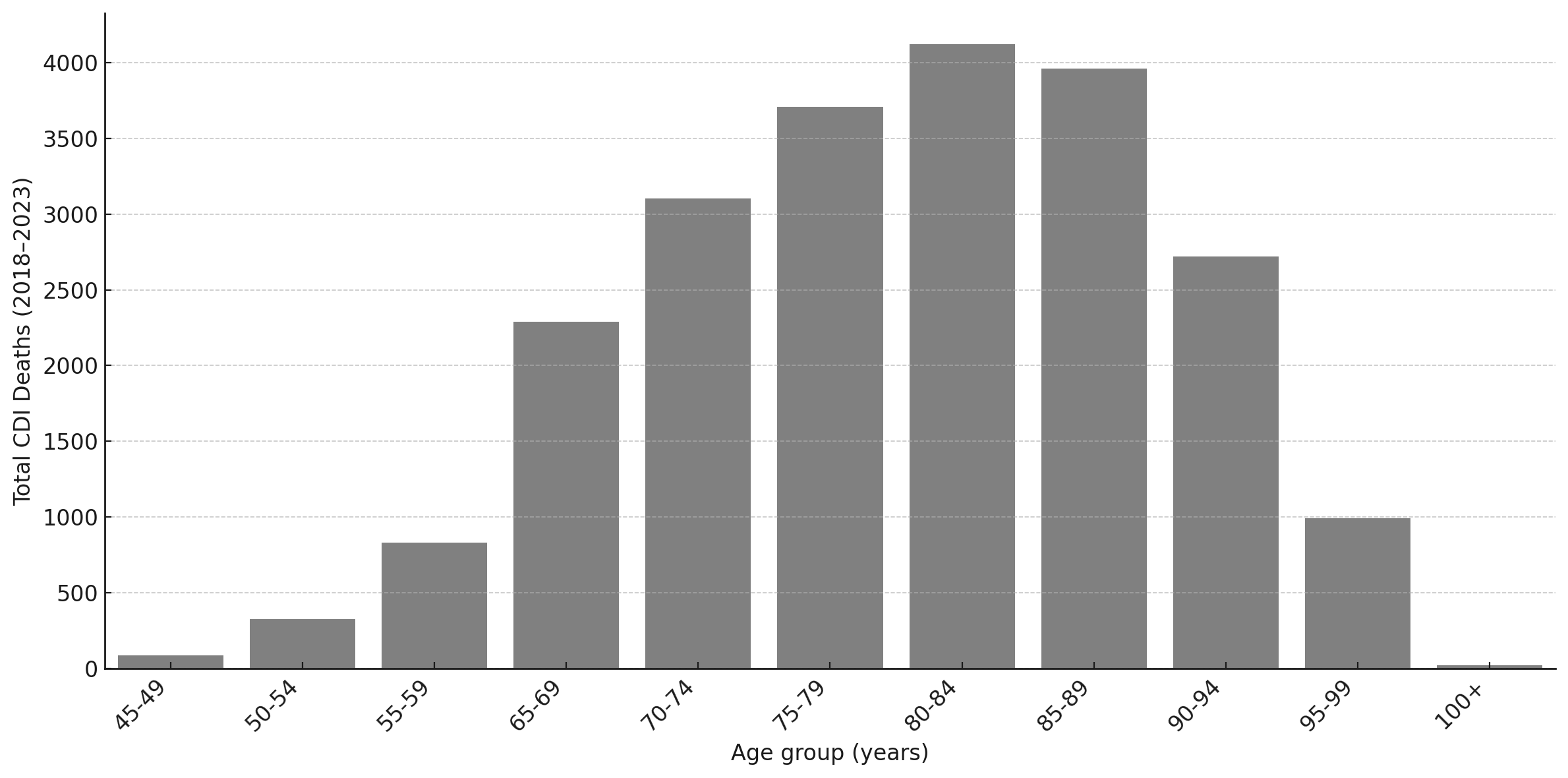
Results: CDI mortality rose more than 10-fold during the pre-therapeutic era (1999–2010), from 599 deaths in 1999 to 6,877 in 2010 (average: 4,055/year). The post-therapeutic era (2011–2023) began with a peak of 7,672 deaths in 2011, followed by a sustained decline to 3,680 deaths/year (average, 2020–2023)- a 52% reduction. Five epidemic phases were observed: early epidemic (1999–2003), peak epidemic (2004–2008), therapeutic transition (2009–2013), post-therapeutic plateau (2014–2018), and recent decline (2019–2023). Among all deaths during 2018–2023, 67% occurred in individuals ≥80 years old, with the 85–89 group representing the largest single demographic (24.9%). Metropolitan areas accounted for 77% of CDI deaths.
Discussion: CDI mortality in the U.S. showed a biphasic pattern, with sharp increases before 2011 and sustained declines thereafter, most notably after 2020. These reductions align with novel therapies and infection prevention efforts. While causality is uncertain, the findings suggest therapeutic and systems-level advances have improved outcomes, especially among elderly patients in metropolitan areas. Future work should disentangle the effects of treatment, prevention, and health system changes.
Disclosures:
John K. Appiah, MD1, George S. Blewusi, MD2, Richeal Asante, MD3, Emmanuel Asare, 4, John Boger, MD1. P1309 - Declining Mortality From <i>Clostridioides difficile</i> Infection Following Therapeutic Innovation: A 25-Year National Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2Johns Hopkins Bloomberg School of Public Health, Baltimore, MD; 3Geisinger Wyoming Valley Medical Center, Kingston, PA; 4Montefiore hospital, Bronx, NY
Introduction: The introduction of fidaxomicin, bezlotoxumab, and fecal microbiota-based therapies marks a new era in the management of Clostridioides difficile infection (CDI). However, the impact of these therapeutic advances on population-level CDI-associated mortality remains unclear. This study evaluates national trends in CDI mortality before and after their introduction, with secondary analyses by age group and geographic setting.
Methods: CDC WONDER Multiple Cause of Death data (1999–2023) were used to identify all deaths listing CDI as a cause. Crude mortality rates per 100,000 population were calculated annually and summarized in five-year intervals. The post-therapeutic era was defined as beginning in 2011, corresponding to the approval of fidaxomicin. Mortality was further stratified by five-year age groups and urban-rural status using the 2013 NCHS Urban-Rural Classification.
Results: CDI mortality rose more than 10-fold during the pre-therapeutic era (1999–2010), from 599 deaths in 1999 to 6,877 in 2010 (average: 4,055/year). The post-therapeutic era (2011–2023) began with a peak of 7,672 deaths in 2011, followed by a sustained decline to 3,680 deaths/year (average, 2020–2023)- a 52% reduction. Five epidemic phases were observed: early epidemic (1999–2003), peak epidemic (2004–2008), therapeutic transition (2009–2013), post-therapeutic plateau (2014–2018), and recent decline (2019–2023). Among all deaths during 2018–2023, 67% occurred in individuals ≥80 years old, with the 85–89 group representing the largest single demographic (24.9%). Metropolitan areas accounted for 77% of CDI deaths.
Discussion: CDI mortality in the U.S. showed a biphasic pattern, with sharp increases before 2011 and sustained declines thereafter, most notably after 2020. These reductions align with novel therapies and infection prevention efforts. While causality is uncertain, the findings suggest therapeutic and systems-level advances have improved outcomes, especially among elderly patients in metropolitan areas. Future work should disentangle the effects of treatment, prevention, and health system changes.
Figure: Figure 1. Annual CDI-associated deaths in the United States, 1999–2023.
Total deaths where CDI was listed as a cause, based on CDC WONDER data. The red dashed line marks the beginning of the therapeutic era in 2011, corresponding to the approval of fidaxomicin and introduction of other novel therapies.
Total deaths where CDI was listed as a cause, based on CDC WONDER data. The red dashed line marks the beginning of the therapeutic era in 2011, corresponding to the approval of fidaxomicin and introduction of other novel therapies.
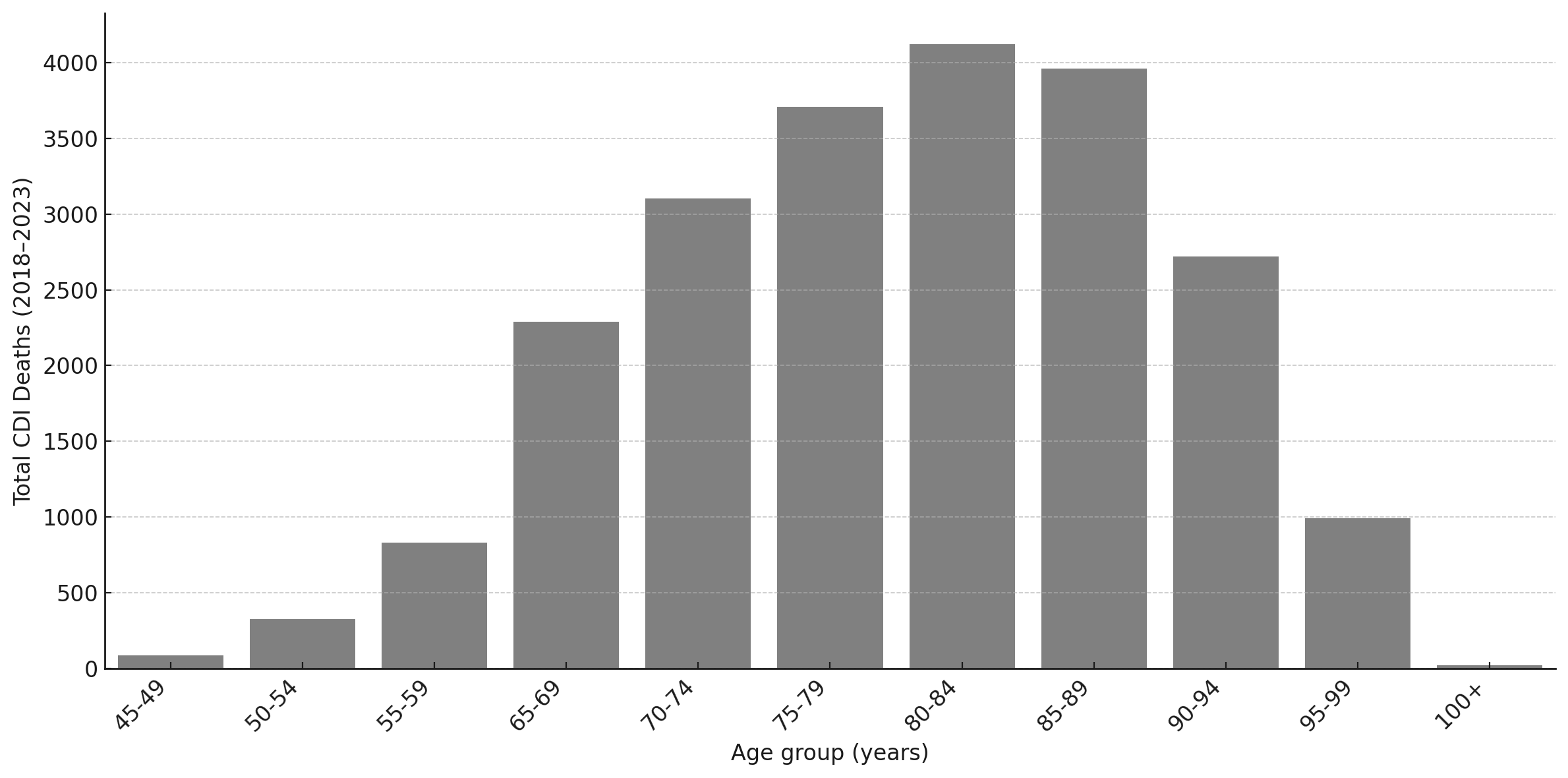
Figure: Figure 2. Age-stratified CDI-associated deaths in the United States, 2018–2023.
Total CDI deaths by five-year age group. The burden of mortality increases sharply with age, with the 85–89 age group representing the single largest demographic, accounting for 24.9% of deaths.
Total CDI deaths by five-year age group. The burden of mortality increases sharply with age, with the 85–89 age group representing the single largest demographic, accounting for 24.9% of deaths.
Disclosures:
John Appiah indicated no relevant financial relationships.
George Blewusi indicated no relevant financial relationships.
Richeal Asante indicated no relevant financial relationships.
Emmanuel Asare indicated no relevant financial relationships.
John Boger indicated no relevant financial relationships.
John K. Appiah, MD1, George S. Blewusi, MD2, Richeal Asante, MD3, Emmanuel Asare, 4, John Boger, MD1. P1309 - Declining Mortality From <i>Clostridioides difficile</i> Infection Following Therapeutic Innovation: A 25-Year National Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
