Sunday Poster Session
Category: Infections and Microbiome
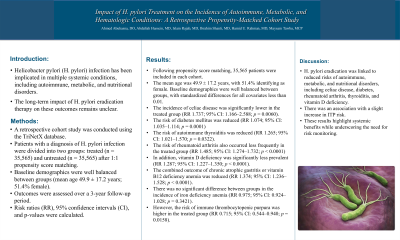
P1310 - Impact of H. pylori Treatment on the Incidence of Autoimmune, Metabolic, and Hematologic Conditions: A Retrospective Propensity-Matched Cohort Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Has Audio
Ahmed Abuhasna, DO
Advocate Illinois Masonic Medical Center
Chicago, IL
Presenting Author(s)
Ahmed Abuhasna, DO1, Abdallah Hussein, MD2, Islam Rajab, MD3, Ibrahim Shanti, MD4, Hamid U.. Rahman, MD1, Maysam Tawba, MCP5, Abdalhakim Shubietah, MD1
1Advocate Illinois Masonic Medical Center, Chicago, IL; 2Virtua Our Lady of Lourdes Hospital, Camden, NJ; 3St. Joseph's University Medical Center, Paterson, NJ; 4Marshall University - - Huntington, WV, Huntington, WV; 5Al Qassimi Women's and Children's Hospital, Sharjah, Sharjah, United Arab Emirates
Introduction: Helicobacter pylori (H. pylori) infection has been implicated in multiple systemic conditions, including autoimmune, metabolic, and nutritional disorders. However, the long-term impact of H. pylori eradication therapy on these outcomes remains unclear.
Methods: A retrospective cohort study was conducted using the TriNetX database. Patients with a diagnosis of H. pylori infection were divided into two groups: treated (n = 35,565) and untreated (n = 35,565) after 1:1 propensity score matching. Baseline demographics were well balanced between groups (mean age 49.9 ± 17.2 years; 51.4% female). Outcomes were assessed over a 3-year follow-up period. Risk ratios (RR), 95% confidence intervals (CI), and p-values were calculated.
Results: Following propensity score matching, 35,565 patients were included in each cohort. The mean age was 49.9 ± 17.2 years, with 51.4% identifying as female. Baseline demographics were well balanced between groups, with standardized differences for all covariates less than 0.01.
The incidence of celiac disease was significantly lower in the treated group (RR 1.737; 95% CI: 1.166–2.588; p = 0.0060). Similarly, the risk of diabetes mellitus was reduced (RR 1.074; 95% CI: 1.035–1.114; p = 0.0001), as was the risk of autoimmune thyroiditis (RR 1.265; 95% CI: 1.021–1.570; p = 0.0322). Rheumatoid arthritis also occurred less frequently in the treated group (RR 1.485; 95% CI: 1.274–1.732; p < 0.0001).
In addition, vitamin D deficiency was significantly less prevalent (RR 1.287; 95% CI: 1.227–1.350; p < 0.0001), and the combined outcome of chronic atrophic gastritis or vitamin B12 deficiency anemia was reduced (RR 1.374; 95% CI: 1.236–1.528; p < 0.0001).
There was no significant difference between groups in the incidence of iron deficiency anemia (RR 0.975; 95% CI: 0.924–1.028; p = 0.3421). However, the risk of immune thrombocytopenic purpura was higher in the treated group (RR 0.715; 95% CI: 0.544–0.940; p = 0.0158).
Discussion: H. pylori eradication was linked to reduced risks of autoimmune, metabolic, and nutritional disorders, including celiac disease, diabetes, rheumatoid arthritis, thyroiditis, and vitamin D deficiency, but was associated with a slight increase in ITP risk. These results highlight systemic benefits while underscoring the need for risk monitoring.
Disclosures:
Ahmed Abuhasna, DO1, Abdallah Hussein, MD2, Islam Rajab, MD3, Ibrahim Shanti, MD4, Hamid U.. Rahman, MD1, Maysam Tawba, MCP5, Abdalhakim Shubietah, MD1. P1310 - Impact of <i>H. pylori</i> Treatment on the Incidence of Autoimmune, Metabolic, and Hematologic Conditions: A Retrospective Propensity-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Advocate Illinois Masonic Medical Center, Chicago, IL; 2Virtua Our Lady of Lourdes Hospital, Camden, NJ; 3St. Joseph's University Medical Center, Paterson, NJ; 4Marshall University - - Huntington, WV, Huntington, WV; 5Al Qassimi Women's and Children's Hospital, Sharjah, Sharjah, United Arab Emirates
Introduction: Helicobacter pylori (H. pylori) infection has been implicated in multiple systemic conditions, including autoimmune, metabolic, and nutritional disorders. However, the long-term impact of H. pylori eradication therapy on these outcomes remains unclear.
Methods: A retrospective cohort study was conducted using the TriNetX database. Patients with a diagnosis of H. pylori infection were divided into two groups: treated (n = 35,565) and untreated (n = 35,565) after 1:1 propensity score matching. Baseline demographics were well balanced between groups (mean age 49.9 ± 17.2 years; 51.4% female). Outcomes were assessed over a 3-year follow-up period. Risk ratios (RR), 95% confidence intervals (CI), and p-values were calculated.
Results: Following propensity score matching, 35,565 patients were included in each cohort. The mean age was 49.9 ± 17.2 years, with 51.4% identifying as female. Baseline demographics were well balanced between groups, with standardized differences for all covariates less than 0.01.
The incidence of celiac disease was significantly lower in the treated group (RR 1.737; 95% CI: 1.166–2.588; p = 0.0060). Similarly, the risk of diabetes mellitus was reduced (RR 1.074; 95% CI: 1.035–1.114; p = 0.0001), as was the risk of autoimmune thyroiditis (RR 1.265; 95% CI: 1.021–1.570; p = 0.0322). Rheumatoid arthritis also occurred less frequently in the treated group (RR 1.485; 95% CI: 1.274–1.732; p < 0.0001).
In addition, vitamin D deficiency was significantly less prevalent (RR 1.287; 95% CI: 1.227–1.350; p < 0.0001), and the combined outcome of chronic atrophic gastritis or vitamin B12 deficiency anemia was reduced (RR 1.374; 95% CI: 1.236–1.528; p < 0.0001).
There was no significant difference between groups in the incidence of iron deficiency anemia (RR 0.975; 95% CI: 0.924–1.028; p = 0.3421). However, the risk of immune thrombocytopenic purpura was higher in the treated group (RR 0.715; 95% CI: 0.544–0.940; p = 0.0158).
Discussion: H. pylori eradication was linked to reduced risks of autoimmune, metabolic, and nutritional disorders, including celiac disease, diabetes, rheumatoid arthritis, thyroiditis, and vitamin D deficiency, but was associated with a slight increase in ITP risk. These results highlight systemic benefits while underscoring the need for risk monitoring.
Disclosures:
Ahmed Abuhasna indicated no relevant financial relationships.
Abdallah Hussein indicated no relevant financial relationships.
Islam Rajab indicated no relevant financial relationships.
Ibrahim Shanti indicated no relevant financial relationships.
Hamid Rahman indicated no relevant financial relationships.
Maysam Tawba indicated no relevant financial relationships.
Abdalhakim Shubietah indicated no relevant financial relationships.
Ahmed Abuhasna, DO1, Abdallah Hussein, MD2, Islam Rajab, MD3, Ibrahim Shanti, MD4, Hamid U.. Rahman, MD1, Maysam Tawba, MCP5, Abdalhakim Shubietah, MD1. P1310 - Impact of <i>H. pylori</i> Treatment on the Incidence of Autoimmune, Metabolic, and Hematologic Conditions: A Retrospective Propensity-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
