Sunday Poster Session
Category: Infections and Microbiome
P1311 - From Gut to Guillain-Barre: Recurrent C. difficile Complications Treated With Plasmapheresis and Fecal Transplant
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Has Audio

John Michael Vincent Coralde, MD
Southwest Healthcare MEC
Murrieta, CA
Presenting Author(s)
Award: ACG Presidential Poster Award
John Michael Vincent Coralde, MD1, Youstina Beshay-Taylor, DO2, Jamie Greathouse, DO2, Rabi Bhatta, MD2, Kameron Kishaba, DO2, Min-Kyung Kang, MD2, Indraneel Chakrabarty, MD2
1Southwest Healthcare MEC, Murrieta, CA; 2Southwest Healthcare MEC, Temecula, CA
Introduction: Guillain-Barré syndrome (GBS) is one of the common triggers of acute flaccid palsy and often are associated with multiple pathogens including Campylobacter spp., Cytomegalovirus, Epstein-Barr virus, Haemophilus Influenzae, Mycoplasma Pneumoniae, and Influenza according to Tam et.al. This case highlights the intricate relationship between recurrent Clostridium difficile (C. difficile) infection leading to a case of atypical Guillain-Barré syndrome (GBS).
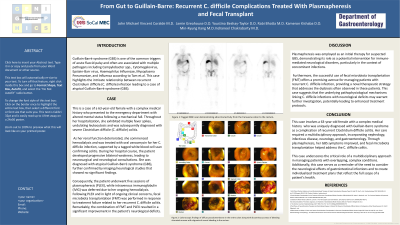
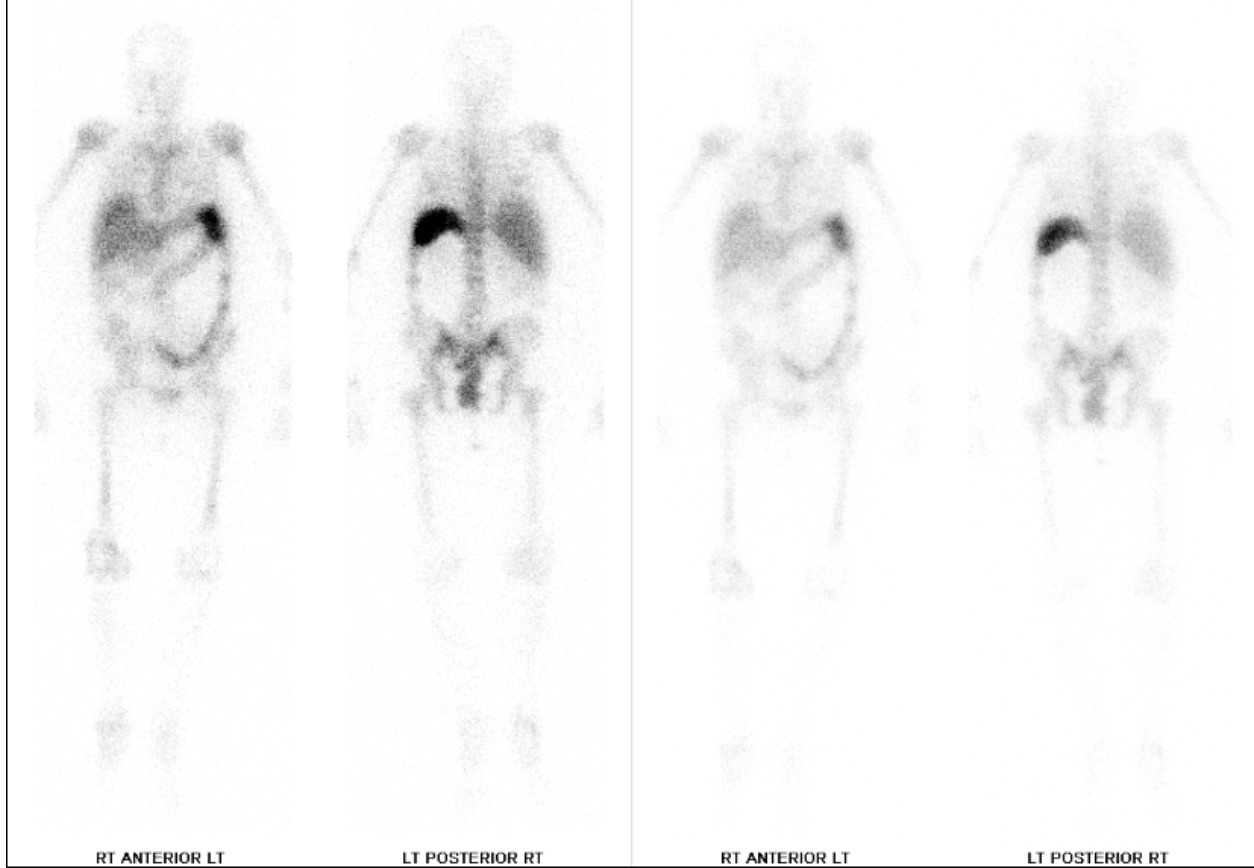
Case Description/Methods: This was a case of a 63-year-old female with a complex medical history who presented to the emergency department with altered mental status following a mechanical fall. Throughout her hospitalization, she exhibited multiple fever spikes, diagnosed with severe Clostridium difficile (C. difficile) colitis. As her renal function deteriorated, she commenced hemodialysis and was treated with oral vancomycin for her C. difficile infection, supported by a tagged white blood cell scan confirming colitis. During her hospital course, the patient developed progressive bilateral weakness, leading to neurosurgical and neurological consultations. She was diagnosed with atypical Guillain-Barré syndrome (GBS), further confirmed by imaging/neurological studies that showed no significant findings. Consequently, the patient underwent five sessions of plasmapheresis (PLEX), while intravenous immunoglobulin (IVIG) was deferred due to her ongoing hemodialysis. Following PLEX and in light of ongoing clinical concerns, fecal microbiota transplantation (FMT) was performed in response to treatment failure related to her recurrent C. difficile colitis. Remarkably, the combination of FMT and PLEX resulted in a significant improvement in the patient's neurological deficits.
Discussion: Plasmapheresis was employed as an initial therapy for suspected GBS, demonstrating its role as a potential intervention for immune-mediated neurological disorders, particularly in the context of concomitant infections. Furthermore, the successful use of fecal microbiota transplantation (FMT) offers a promising avenue for managing patients with recurrent C. difficile infection, providing a novel therapeutic strategy that addresses the dysbiosis often observed in these patients. This case suggests that the underlying pathophysiological mechanisms linking C. difficile infections with neurological deficits may warrant further investigation, potentially leading to enhanced treatment protocols.
Disclosures:
John Michael Vincent Coralde, MD1, Youstina Beshay-Taylor, DO2, Jamie Greathouse, DO2, Rabi Bhatta, MD2, Kameron Kishaba, DO2, Min-Kyung Kang, MD2, Indraneel Chakrabarty, MD2. P1311 - From Gut to Guillain-Barre: Recurrent <i>C. difficile</i> Complications Treated With Plasmapheresis and Fecal Transplant, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
John Michael Vincent Coralde, MD1, Youstina Beshay-Taylor, DO2, Jamie Greathouse, DO2, Rabi Bhatta, MD2, Kameron Kishaba, DO2, Min-Kyung Kang, MD2, Indraneel Chakrabarty, MD2
1Southwest Healthcare MEC, Murrieta, CA; 2Southwest Healthcare MEC, Temecula, CA
Introduction: Guillain-Barré syndrome (GBS) is one of the common triggers of acute flaccid palsy and often are associated with multiple pathogens including Campylobacter spp., Cytomegalovirus, Epstein-Barr virus, Haemophilus Influenzae, Mycoplasma Pneumoniae, and Influenza according to Tam et.al. This case highlights the intricate relationship between recurrent Clostridium difficile (C. difficile) infection leading to a case of atypical Guillain-Barré syndrome (GBS).
Case Description/Methods: This was a case of a 63-year-old female with a complex medical history who presented to the emergency department with altered mental status following a mechanical fall. Throughout her hospitalization, she exhibited multiple fever spikes, diagnosed with severe Clostridium difficile (C. difficile) colitis. As her renal function deteriorated, she commenced hemodialysis and was treated with oral vancomycin for her C. difficile infection, supported by a tagged white blood cell scan confirming colitis. During her hospital course, the patient developed progressive bilateral weakness, leading to neurosurgical and neurological consultations. She was diagnosed with atypical Guillain-Barré syndrome (GBS), further confirmed by imaging/neurological studies that showed no significant findings. Consequently, the patient underwent five sessions of plasmapheresis (PLEX), while intravenous immunoglobulin (IVIG) was deferred due to her ongoing hemodialysis. Following PLEX and in light of ongoing clinical concerns, fecal microbiota transplantation (FMT) was performed in response to treatment failure related to her recurrent C. difficile colitis. Remarkably, the combination of FMT and PLEX resulted in a significant improvement in the patient's neurological deficits.
Discussion: Plasmapheresis was employed as an initial therapy for suspected GBS, demonstrating its role as a potential intervention for immune-mediated neurological disorders, particularly in the context of concomitant infections. Furthermore, the successful use of fecal microbiota transplantation (FMT) offers a promising avenue for managing patients with recurrent C. difficile infection, providing a novel therapeutic strategy that addresses the dysbiosis often observed in these patients. This case suggests that the underlying pathophysiological mechanisms linking C. difficile infections with neurological deficits may warrant further investigation, potentially leading to enhanced treatment protocols.
Figure: Tagged WBC scan demonstrating abnormal activity from the transverse colon to the rectum.
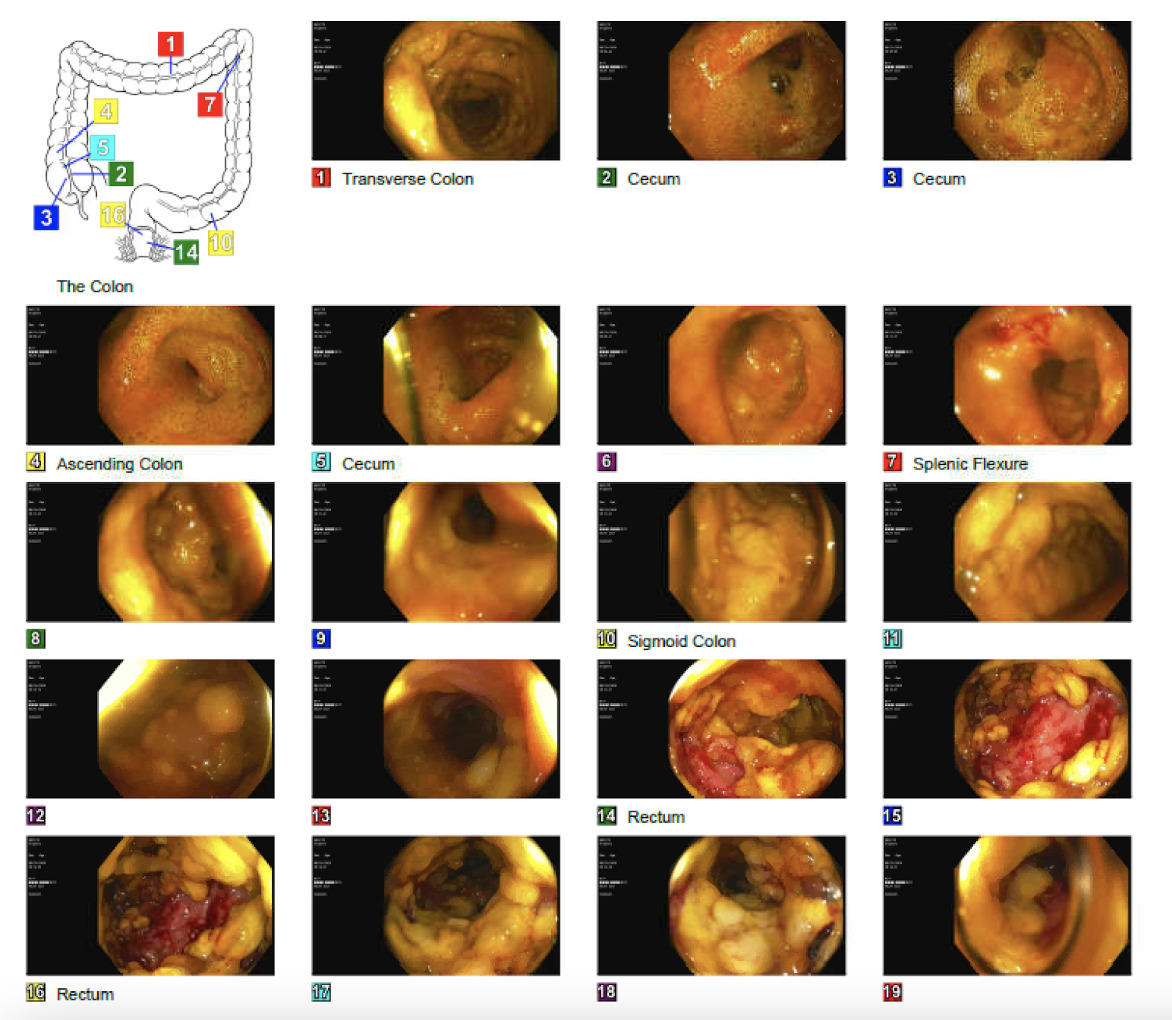
Figure: Colonoscopic findings of diffuse pseudomembrane in the entire colon along with discontinuous areas of bleeding ulcerated mucosa with stigmata of recent bleeding in the rectum.
Disclosures:
John Michael Vincent Coralde indicated no relevant financial relationships.
Youstina Beshay-Taylor indicated no relevant financial relationships.
Jamie Greathouse indicated no relevant financial relationships.
Rabi Bhatta indicated no relevant financial relationships.
Kameron Kishaba indicated no relevant financial relationships.
Min-Kyung Kang indicated no relevant financial relationships.
Indraneel Chakrabarty indicated no relevant financial relationships.
John Michael Vincent Coralde, MD1, Youstina Beshay-Taylor, DO2, Jamie Greathouse, DO2, Rabi Bhatta, MD2, Kameron Kishaba, DO2, Min-Kyung Kang, MD2, Indraneel Chakrabarty, MD2. P1311 - From Gut to Guillain-Barre: Recurrent <i>C. difficile</i> Complications Treated With Plasmapheresis and Fecal Transplant, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

