Sunday Poster Session
Category: Esophagus
P0621 - Increased Risk of Barrett’s Esophagus After Bariatric Surgery: A Propensity-Matched Analysis of 57,035 Patients
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall


Mohamed Eldesouki, MD
Saint Michael's Medical Center, New York Medical College
Newark, NJ
Presenting Author(s)
Mohamed Eldesouki, MD1, Ahmed Ibrahim, MD2, Mohammed Y. Youssef, MD3, Ahmed Salem, MD4, Hazem Abosheaishaa, MD5, Omar Alkasabrah, MD6, Anas A. Elsaka, MD7, Mona A. Ali, MD7, Sherif E. Elhanafi, MD8
1Saint Michael's Medical Center, New York Medical College, Newark, NJ; 2Medical University of South Carolina, Charleston, SC; 3Hunt Regional Medical Center, Greenville, TX; 4Maimonides Medical Center, Brooklyn, NY; 5Mount Sinai West, Icahn School of Medicine at Mount Sinai, Queens, NY; 6Landmark Medical Center, Woonsocket, RI; 7Mansoura University, Mansoura, Ad Daqahliyah, Egypt; 8Texas Tech University Health Sciences Center, El Paso, TX
Introduction: Bariatric surgeries are widely utilized for obesity management, however, their impact on the risk of developing Barrett’s esophagus (BE) remains uncertain. The aim of this study was to evaluate the long-term risk of BE after bariatric surgery using a large real-world cohort.
Methods: A retrospective cohort study was conducted using the TriNetX database (2000–2020). Adult patients >18 years with body-mass index ≥30 kg/m² who underwent bariatric procedures (sleeve gastrostomy and gastric bypass) were identified using CPT© codes. Obese adults who did not undergo bariatric surgeries, and presented to the clinic were identified as a control group. Individuals with pre-existing BE, esophageal adenocarcinoma (EAC), esophagectomy, or other types of gastric surgeries were excluded. Propensity score matching (PSM) (1:1) was conducted, adjusting for demographics and relevant comorbidities. The primary outcome was the risk of BE, while secondary outcomes were the development of EAC, GERD, esophagitis, and new PPI use. Risk ratios (RR) with 95 % confidence intervals (CI) were calculated for each outcome.
Results: A total of 58,910 patients underwent bariatric surgeries (31,228 sleeve, 27,682 gastric bypass), while 1,049,231 patients were in the control group before PSM. After matching, a total of 57,035 patients remained in each group (Table 1).
Bariatric surgery was associated with a higher incidence of Barrett’s esophagus compared to the control group (0.8% vs 0.5%; RR 1.39, 95 % CI 1.207 – 1.618, p< 0.001). Nondysplastic BE was significantly higher in the bariatric surgeries group (0.8 % vs 0.4 %; RR 1.77, 95 % CI 1.38 – 2.27, p< 0.001), however, no significant increases were noted in dysplastic BE (0.07 % vs 0.05 %; RR 1.60, 95 % CI 0.73–3.53), esophageal adenocarcinoma (0.05% vs 0.026%; RR 1.73, 99% CI 0.92 –3.37), and esophagitis (RR 0.78, 95 % CI 0.69– 1.12, p< 0.5).
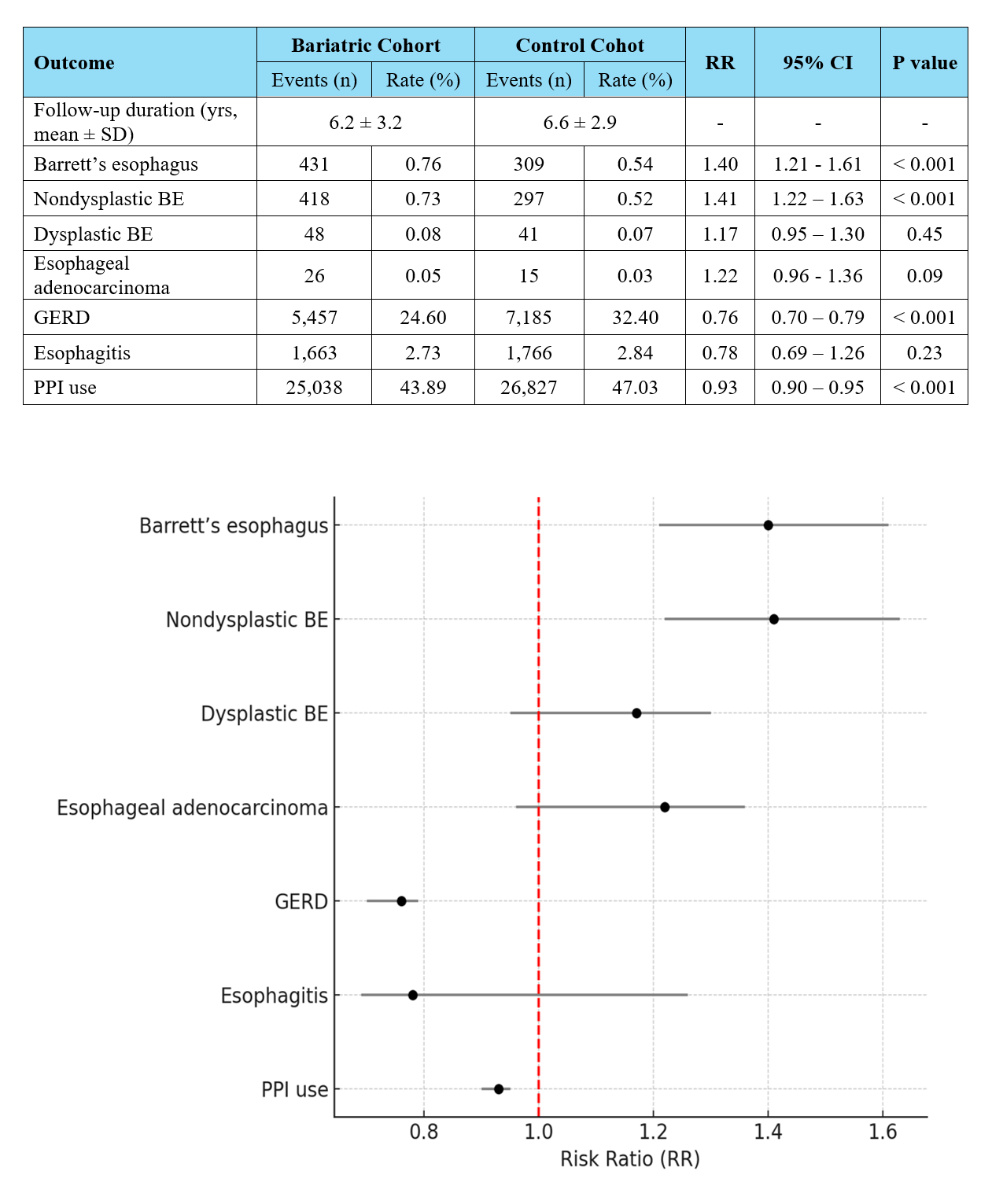
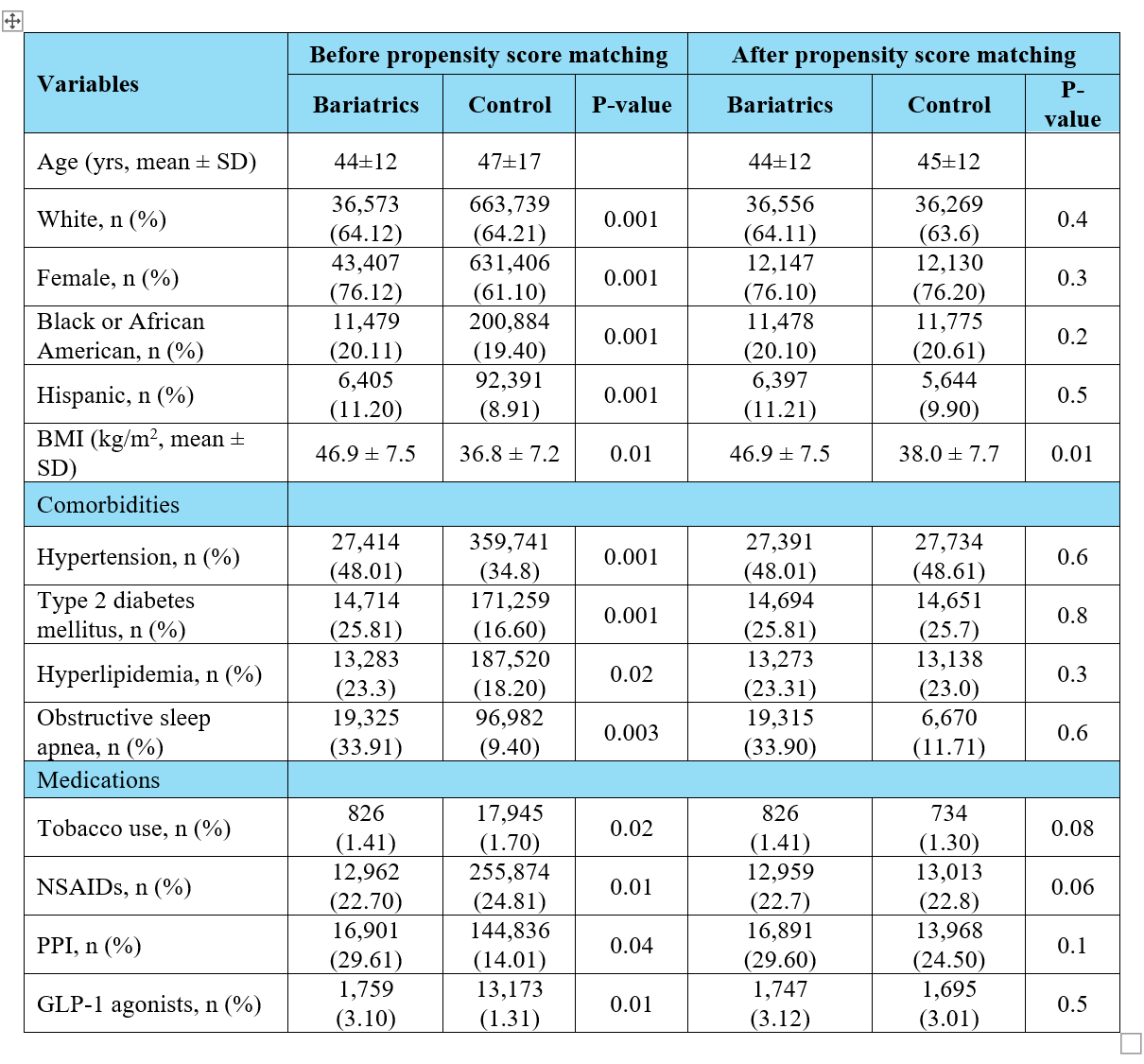
Compared to obese controls, bariatric surgery patients had lower risk of reflux-mediated outcomes: GERD (24.04% vs 26.61%; RR 0.91, 95 % CI 0.84–0.93, p< 0.001), and need for PPI use (35.2 % vs 42.0 %; RR 0.84, 95 % CI 0.81–0.87, p< 0.001) (Table 2, Figure 1).
Discussion: In this large real-world cohort study, the risk of Barrett’s esophagus was higher in patients who underwent bariatric surgeries; however, bariatric surgeries were associated with substantial reductions in the development of GERD and PPI utilization. Prospective studies and tailored surveillance strategies for post-bariatric patients are warranted.
Disclosures:
Mohamed Eldesouki, MD1, Ahmed Ibrahim, MD2, Mohammed Y. Youssef, MD3, Ahmed Salem, MD4, Hazem Abosheaishaa, MD5, Omar Alkasabrah, MD6, Anas A. Elsaka, MD7, Mona A. Ali, MD7, Sherif E. Elhanafi, MD8. P0621 - Increased Risk of Barrett’s Esophagus After Bariatric Surgery: A Propensity-Matched Analysis of 57,035 Patients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Saint Michael's Medical Center, New York Medical College, Newark, NJ; 2Medical University of South Carolina, Charleston, SC; 3Hunt Regional Medical Center, Greenville, TX; 4Maimonides Medical Center, Brooklyn, NY; 5Mount Sinai West, Icahn School of Medicine at Mount Sinai, Queens, NY; 6Landmark Medical Center, Woonsocket, RI; 7Mansoura University, Mansoura, Ad Daqahliyah, Egypt; 8Texas Tech University Health Sciences Center, El Paso, TX
Introduction: Bariatric surgeries are widely utilized for obesity management, however, their impact on the risk of developing Barrett’s esophagus (BE) remains uncertain. The aim of this study was to evaluate the long-term risk of BE after bariatric surgery using a large real-world cohort.
Methods: A retrospective cohort study was conducted using the TriNetX database (2000–2020). Adult patients >18 years with body-mass index ≥30 kg/m² who underwent bariatric procedures (sleeve gastrostomy and gastric bypass) were identified using CPT© codes. Obese adults who did not undergo bariatric surgeries, and presented to the clinic were identified as a control group. Individuals with pre-existing BE, esophageal adenocarcinoma (EAC), esophagectomy, or other types of gastric surgeries were excluded. Propensity score matching (PSM) (1:1) was conducted, adjusting for demographics and relevant comorbidities. The primary outcome was the risk of BE, while secondary outcomes were the development of EAC, GERD, esophagitis, and new PPI use. Risk ratios (RR) with 95 % confidence intervals (CI) were calculated for each outcome.
Results: A total of 58,910 patients underwent bariatric surgeries (31,228 sleeve, 27,682 gastric bypass), while 1,049,231 patients were in the control group before PSM. After matching, a total of 57,035 patients remained in each group (Table 1).
Bariatric surgery was associated with a higher incidence of Barrett’s esophagus compared to the control group (0.8% vs 0.5%; RR 1.39, 95 % CI 1.207 – 1.618, p< 0.001). Nondysplastic BE was significantly higher in the bariatric surgeries group (0.8 % vs 0.4 %; RR 1.77, 95 % CI 1.38 – 2.27, p< 0.001), however, no significant increases were noted in dysplastic BE (0.07 % vs 0.05 %; RR 1.60, 95 % CI 0.73–3.53), esophageal adenocarcinoma (0.05% vs 0.026%; RR 1.73, 99% CI 0.92 –3.37), and esophagitis (RR 0.78, 95 % CI 0.69– 1.12, p< 0.5).
Compared to obese controls, bariatric surgery patients had lower risk of reflux-mediated outcomes: GERD (24.04% vs 26.61%; RR 0.91, 95 % CI 0.84–0.93, p< 0.001), and need for PPI use (35.2 % vs 42.0 %; RR 0.84, 95 % CI 0.81–0.87, p< 0.001) (Table 2, Figure 1).
Discussion: In this large real-world cohort study, the risk of Barrett’s esophagus was higher in patients who underwent bariatric surgeries; however, bariatric surgeries were associated with substantial reductions in the development of GERD and PPI utilization. Prospective studies and tailored surveillance strategies for post-bariatric patients are warranted.
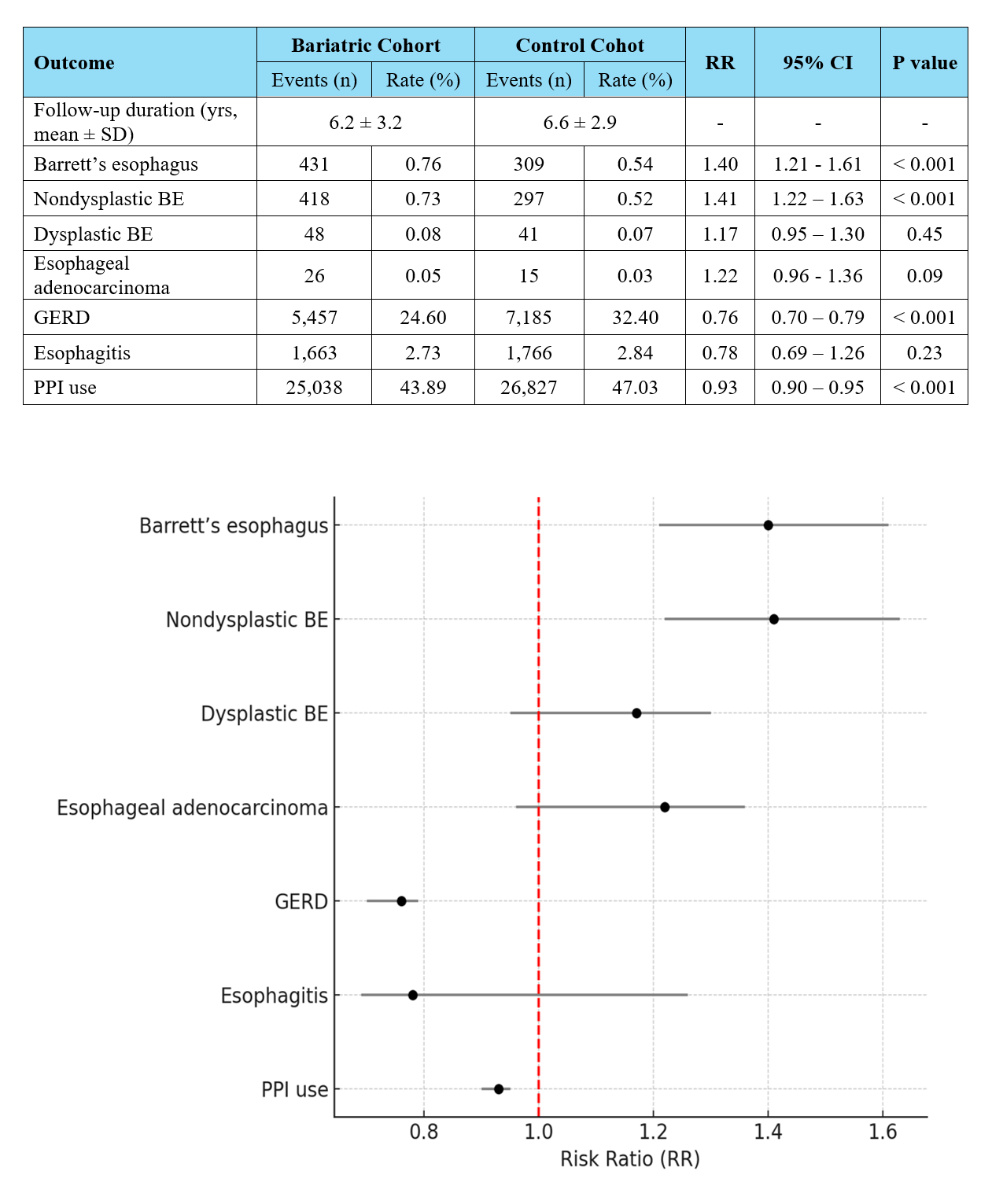
Figure: Table 1. Patients' demographics and clinical features before and after propensity score matching.
Abbreviations- BMI: body mass index; NSAIDs: non-steroidal anti-inflammatory drugs; PPI: proton pump inhibitors; GLP-1: glucagon-like peptide-1.
Abbreviations- BMI: body mass index; NSAIDs: non-steroidal anti-inflammatory drugs; PPI: proton pump inhibitors; GLP-1: glucagon-like peptide-1.
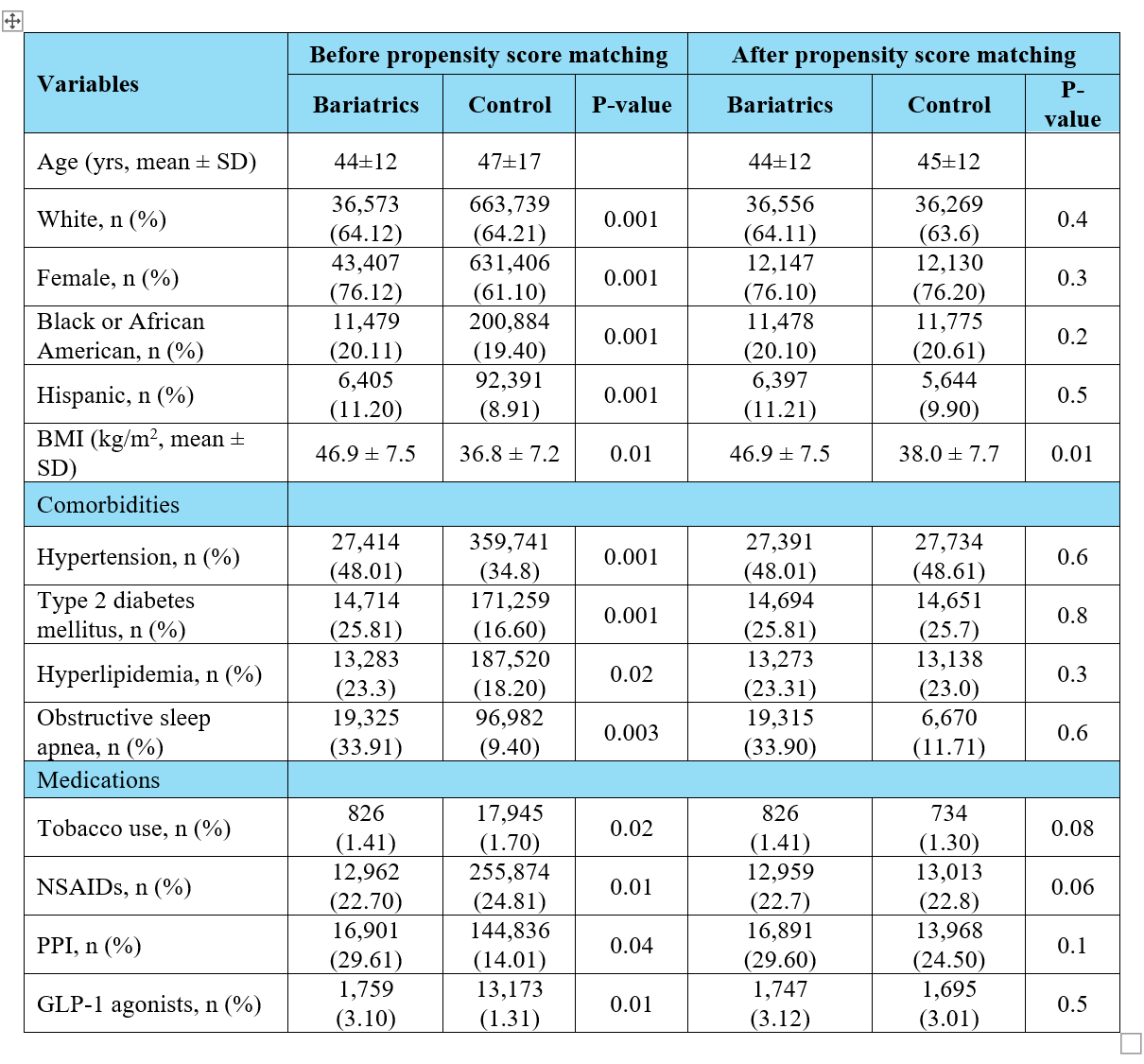
Figure: Table 2. Clinical outcomes of the baratric surgery cohort vs. control.
Figure. Forest plot depicting the clinical outcomes of the bariatric surgery group compared to the control.
Abbreviations- BE: Barrett's esophagus; GERD: gastroesophageal reflux disease; PPI: proton pump inhibitors
Figure. Forest plot depicting the clinical outcomes of the bariatric surgery group compared to the control.
Abbreviations- BE: Barrett's esophagus; GERD: gastroesophageal reflux disease; PPI: proton pump inhibitors
Disclosures:
Mohamed Eldesouki indicated no relevant financial relationships.
Ahmed Ibrahim indicated no relevant financial relationships.
Mohammed Y. Youssef indicated no relevant financial relationships.
Ahmed Salem indicated no relevant financial relationships.
Hazem Abosheaishaa indicated no relevant financial relationships.
Omar Alkasabrah indicated no relevant financial relationships.
Anas Elsaka indicated no relevant financial relationships.
Mona Ali indicated no relevant financial relationships.
Sherif Elhanafi indicated no relevant financial relationships.
Mohamed Eldesouki, MD1, Ahmed Ibrahim, MD2, Mohammed Y. Youssef, MD3, Ahmed Salem, MD4, Hazem Abosheaishaa, MD5, Omar Alkasabrah, MD6, Anas A. Elsaka, MD7, Mona A. Ali, MD7, Sherif E. Elhanafi, MD8. P0621 - Increased Risk of Barrett’s Esophagus After Bariatric Surgery: A Propensity-Matched Analysis of 57,035 Patients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
