Sunday Poster Session
Category: Colon
P0440 - Primary Mixed Neuroendocrine Non-Neuroendocrine Tumor of the Descending Colon With Liver Metastases

Nathan Einhorn, MD
University of South Florida Morsani College of Medicine
Tampa, FL
Presenting Author(s)
1University of South Florida Morsani College of Medicine, Tampa, FL; 2University of South Florida Morsani College of Medicine and James A. Haley VA Hospital, Tampa, FL
Introduction:
Mixed neuroendocrine non-neuroendocrine neoplasms (MiNENs) are a group of rare malignancies composed of both neuroendocrine and non-neuroendocrine components, each representing at least 30% of the tumor volume. Colorectal MiNENs are an aggressive subset with unfavorable outcomes. Here, we report a case of colonic MiNEN with liver metastases to illustrate the diagnostic complexity and poor prognosis of these tumors.
Case Description/Methods:
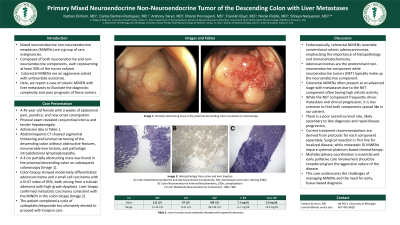
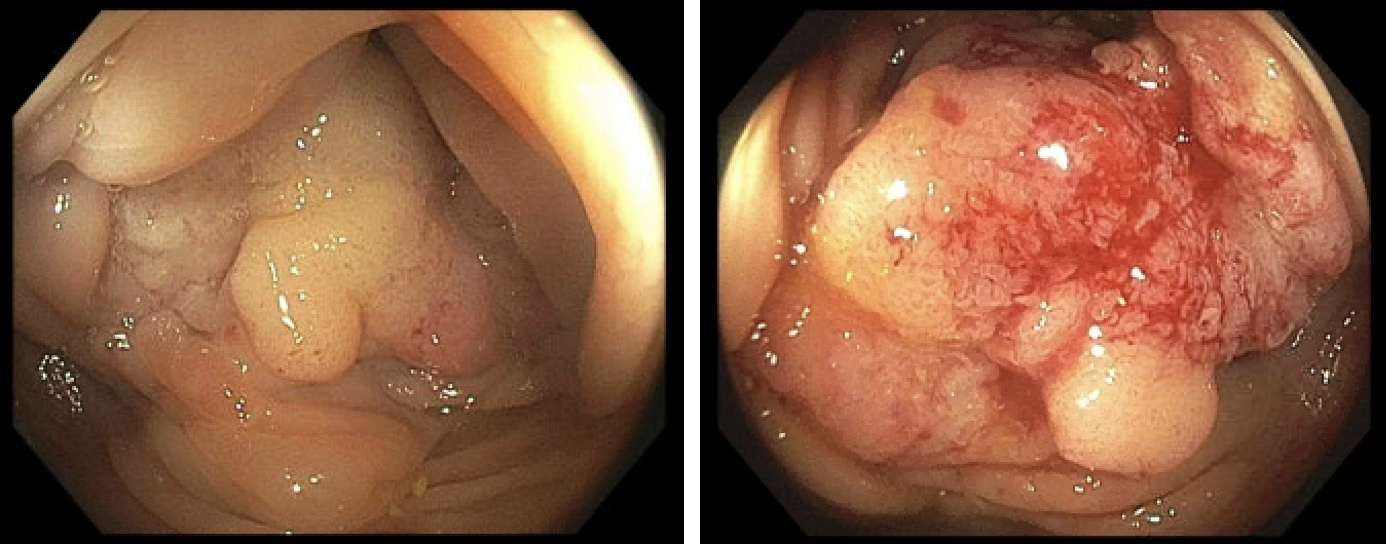
A 45-year-old female presented with 3 weeks of abdominal pain, jaundice, and new-onset constipation. Physical exam revealed conjunctival icterus and tender hepatomegaly. Admission labs were notable for AST 212 U/L, ALT 87 U/L, alkaline phosphatase 584 IU/L, and total bilirubin 7.1 mg/dL (conjugated 5.8 mg/dL). Abdominopelvic CT showed segmental thickening and luminal narrowing of the descending colon without obstructive features, innumerable liver lesions, and pathologic intra-abdominal lymphadenopathy. A 4 cm partially obstructing mass was found in the proximal descending colon on subsequent colonoscopy (Image 1). Biopsies thereof showed moderately differentiated adenocarcinoma and a small cell carcinoma with a Ki-67 index of 95%, both arising from a tubular adenoma with high-grade dysplasia. Biopsies of the liver lesions confirmed metastatic carcinoma, consistent with the MiNEN present in the colon biopsy (Image 2). The patient completed a cycle of carboplatin/etoposide but ultimately elected to proceed with hospice care.
Discussion:
Endoscopically, colorectal MiNENs resemble conventional colonic adenocarcinomas emphasizing the importance of histopathology and immunohistochemistry. Adenocarcinomas are the predominant non-neuroendocrine component while neuroendocrine tumors (NET) typically make up the neuroendocrine component. Colorectal MiNENs often present at an advanced stage with metastases due to the NET component frequently having high mitotic activity. While the NET component often drives metastasis and clinical progression, it is less common to find both components spread like in our patient. There is a poor overall survival rate, likely secondary to late diagnoses and rapid disease progression. Current treatment recommendations are derived from protocols for each component separately. Surgical resection is first line for localized disease, while metastatic GI MiNENs require systemic platinum-based chemotherapy. This case underscores the challenges of managing MiNENs and the need for early, tissue-based diagnosis.
Disclosures:
Nathan Einhorn, MD1, Carlos Bertran-Rodriguez, MD1, Anthony Skryd, MD1, Bharat Ponnaganti, MD1, Franklin Boyd, MD1, Nicole Riddle, MD1, Shreya Narayanan, MD2. P0440 - Primary Mixed Neuroendocrine Non-Neuroendocrine Tumor of the Descending Colon With Liver Metastases, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
